Post-Approval Changes: What Happens After a Drug Gets Approved
When a drug gets approved by the FDA or EMA, it’s not the end of the story—it’s just the beginning. Post-approval changes, modifications made to a medication after it’s on the market to improve safety, manufacturing, or labeling. Also known as post-marketing changes, these updates can range from tiny tweaks in pill color to major shifts in who can use the drug. Many people assume once a drug is approved, it’s locked in place. But the truth is, manufacturers can—and often do—change ingredients, dosing, packaging, and even how the drug is made. These aren’t random updates. They’re tracked, reviewed, and sometimes required by regulators to fix problems or make things better.
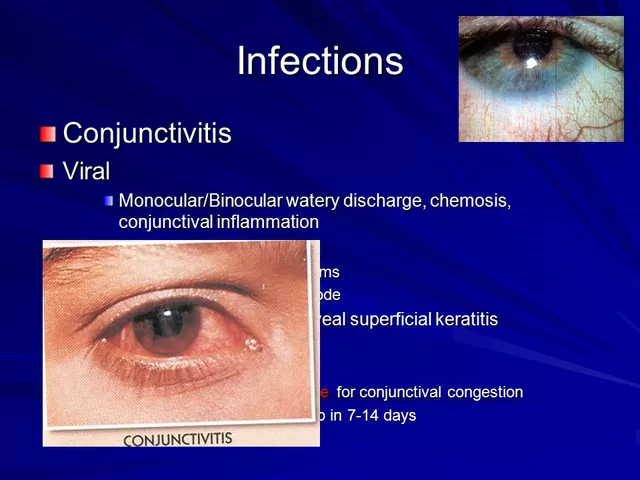
One big reason post-approval changes happen is because real-world use reveals things clinical trials never caught. A drug might work great in a controlled study with 500 people, but what happens when 5 million people take it? Side effects show up. Interactions with other meds become clear. Some patients can’t swallow the pill, so the company makes a liquid version. Or maybe a new factory starts making it, and the formula needs tweaking to match quality standards. These aren’t just paperwork changes—they directly affect your health. A change in the inactive ingredients, for example, could trigger an allergy in someone who never had one before. Or a shift in manufacturing could alter how fast the drug gets into your bloodstream.
Regulators rely on pharmacovigilance, the science of monitoring drug safety after approval to catch these issues. Systems like the FDA’s FAERS database collect reports from doctors, patients, and pharmacies. If a pattern emerges—say, more people report dizziness after a certain batch—investigations start. That’s how changes get triggered. Sometimes, the change is simple: a new warning on the label. Other times, it’s a full recall or a switch to a different manufacturer. Regulatory updates, official decisions made by health authorities to modify drug approvals based on new data are how these fixes get enforced. And while most changes are harmless or even helpful, some can catch patients off guard. You might notice your pill looks different, or your pharmacy switches brands without telling you. That’s often a post-approval change in action.
These updates don’t just affect patients—they impact pharmacists, doctors, and hospitals too. A change in dosage form might mean nurses need new training. A new generic version could alter how insurance covers the drug. That’s why staying informed matters. If you’re on a long-term medication, don’t assume it’s the same as when you started. Check the label. Ask your pharmacist if anything changed. And if you feel different after a switch, speak up. Many of the posts below dive into real cases where small changes had big consequences—from cholesterol meds that stopped working after a formula tweak, to antibiotics with new warnings after years on the shelf. You’ll find stories about how manufacturers, regulators, and patients all play a role in making sure drugs stay safe long after they’re approved.