Injectable Drug Shortages: What’s Happening and How It Affects Your Care
When injectable drug shortages, a situation where hospitals and pharmacies can’t get enough IV or injected medications to meet patient needs. Also known as IV drug shortages, it happens when manufacturers can’t produce enough of a critical medicine—like antibiotics, chemotherapy agents, or anesthetics—to keep up with demand. This isn’t just a supply chain hiccup. It’s a direct threat to patient safety. Think about someone needing an IV antibiotic for a serious infection, or a cancer patient waiting for their life-saving chemo. When those drugs vanish from shelves, doctors have to scramble—switching to less effective options, delaying treatments, or using riskier alternatives.
These shortages aren’t random. They’re tied to manufacturing changes, adjustments in how drugs are made that trigger FDA reviews and can halt production for months. A single factory shutdown—due to quality issues, inspections, or equipment failure—can knock out 80% of the nation’s supply of a common injectable. And because many of these drugs are cheap generics, companies have little incentive to invest in backup production. When demand spikes, like during a flu season or a hospital outbreak, there’s no reserve. You’re left with generic injectables, low-cost versions of brand-name injected drugs that make up most of the market but have fragile supply chains running on empty.
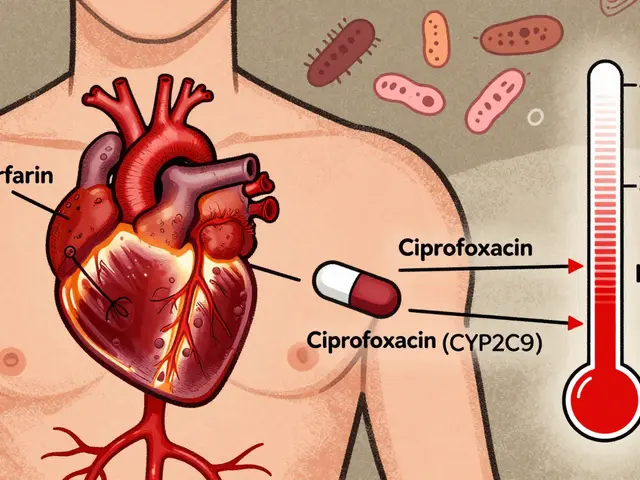
It’s not just about running out of medicine. It’s about what happens next. Nurses might have to dilute doses incorrectly. Doctors may prescribe drugs they’re less familiar with, increasing the risk of side effects. Patients end up waiting longer in ERs, or worse—getting less effective treatment. The FDA tracks these shortages, but their list is always behind the real-time crisis. What you see reported as a "temporary" shortage might already be a three-month delay in your local hospital.
What’s in this collection? Real stories from providers who’ve had to make tough calls when their IV meds disappeared. Guides on how to spot signs of a shortage before it hits your prescription. And clear breakdowns of which injectables are most at risk right now—like vancomycin, phenytoin, and propofol—and what alternatives actually work. You’ll also find advice on how to talk to your doctor if your medication suddenly changes, and what questions to ask when you’re handed a new vial you’ve never seen before.
This isn’t theoretical. If you or someone you care for relies on injectable drugs, you’re already feeling the ripple effect. The goal here isn’t to scare you—it’s to arm you with facts, so you can ask the right questions, recognize when something’s off, and push back when your care is compromised.