Tricyclic Antidepressants: What They Are, How They Work, and What You Need to Know
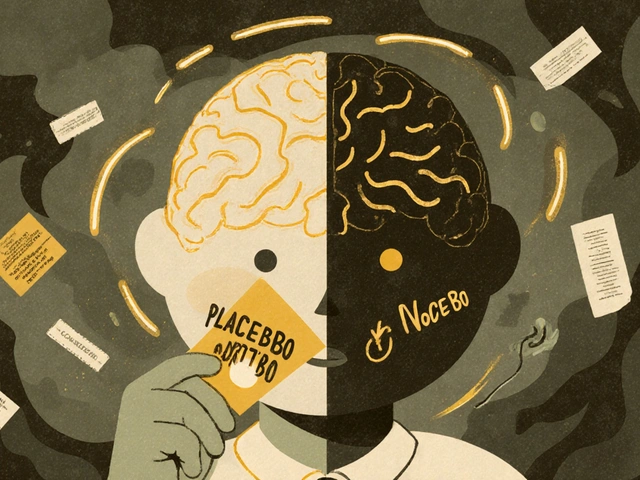
When we talk about tricyclic antidepressants, a class of prescription medications first developed in the 1950s to treat depression by balancing brain chemicals like serotonin and norepinephrine. Also known as TCAs, they were the go-to treatment before SSRIs became popular—but they’re still prescribed today for depression, nerve pain, and even chronic migraines. Unlike newer antidepressants, tricyclics affect multiple brain receptors at once, which is why they work for some people when other drugs don’t. But that same broad action is also why side effects like dry mouth, drowsiness, weight gain, and dizziness are so common.
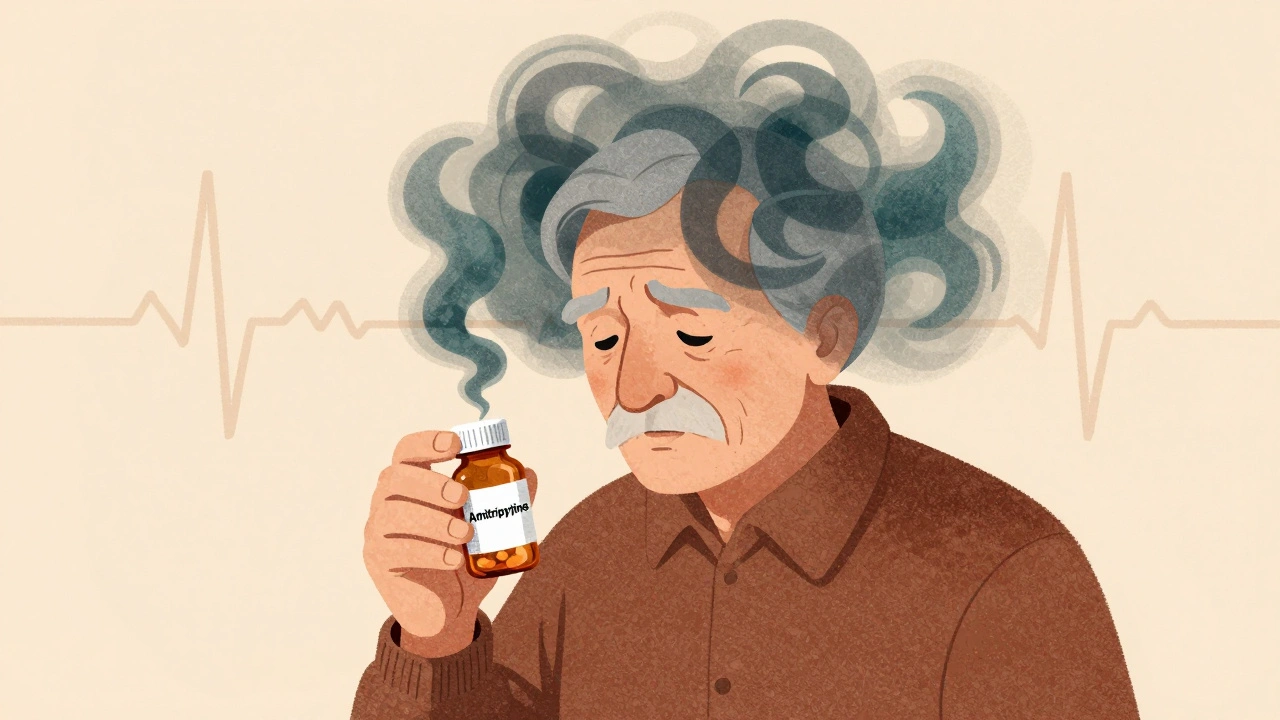
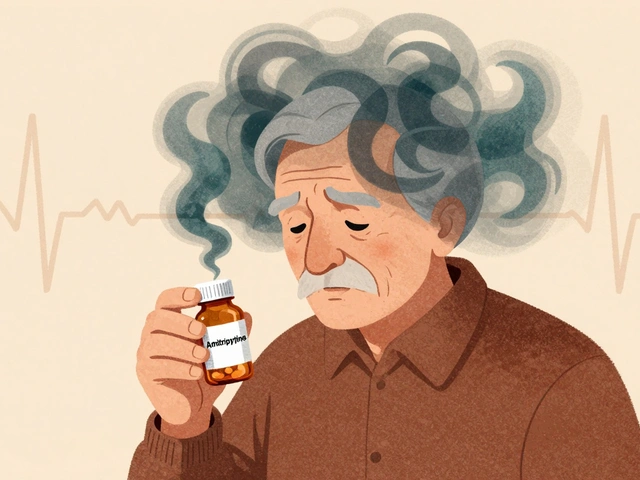
These drugs don’t just target mood—they can influence heart rhythm, blood pressure, and digestion. That’s why adverse drug events, serious unintended reactions to medications that can require emergency care are more likely with tricyclics than with newer options. Over a million emergency visits each year in the U.S. are tied to medication errors or reactions, and older antidepressants like amitriptyline or nortriptyline top the list for preventable harm in older adults. Even small mistakes—like mixing them with alcohol or certain painkillers—can lead to dangerous drops in blood pressure or irregular heartbeats.
What makes tricyclic antidepressants different isn’t just how they work, but who uses them. Many patients turn to them after other treatments fail. Some doctors still prescribe them for chronic pain conditions like fibromyalgia or diabetic neuropathy because they block pain signals in the spinal cord. But they’re not for everyone. People with heart problems, glaucoma, or an enlarged prostate often can’t take them safely. And if you’re over 65, the risks rise fast. Studies show that seniors on TCAs are more likely to fall, get confused, or end up in the hospital than those on newer antidepressants.
There’s also the issue of how these drugs interact with other medications. For example, if you’re taking something like metronidazole, an antibiotic that can interfere with how the liver breaks down other drugs, combining it with a tricyclic antidepressant can spike blood levels and increase side effects. Or if you’re on a blood thinner like warfarin, the way TCAs affect liver enzymes can throw off your INR levels. These aren’t theoretical risks—they show up in real patient stories and hospital data.
What you won’t find in most drug brochures is how people actually experience these meds. Some swear they saved their life. Others describe months of feeling like a zombie, fighting constipation, or waking up with a racing heart. The truth is, tricyclic antidepressants aren’t one-size-fits-all. They require careful monitoring, slow dose adjustments, and honest conversations with your doctor about what you’re feeling—not just whether your mood improved.
Below, you’ll find real-world insights from patients and providers who’ve navigated these drugs—what worked, what didn’t, and what hidden dangers to watch for. Whether you’re considering tricyclics, already taking them, or just trying to understand why your loved one’s prescription changed, this collection gives you the facts without the fluff.