When you pick up a prescription, you might see two options: the name you recognize from TV ads, or a cheaper version with a plain label. You’ve probably wondered - is the generic just as good? Or are you risking your health by saving money?
The short answer? For most people, generic drugs are just as safe and effective as their brand-name counterparts. But it’s not that simple. There are exceptions. And those exceptions matter.
What makes a generic drug "equivalent"?
Generic drugs aren’t knockoffs. They’re legally required to contain the exact same active ingredient, in the same strength, and delivered the same way - whether it’s a pill, injection, or inhaler. The U.S. Food and Drug Administration (FDA) doesn’t approve a generic unless it meets strict standards. The drug must be pharmaceutically equivalent - meaning same active ingredient, same dose, same form. And it must be bioequivalent - meaning your body absorbs it at nearly the same rate and amount as the brand.
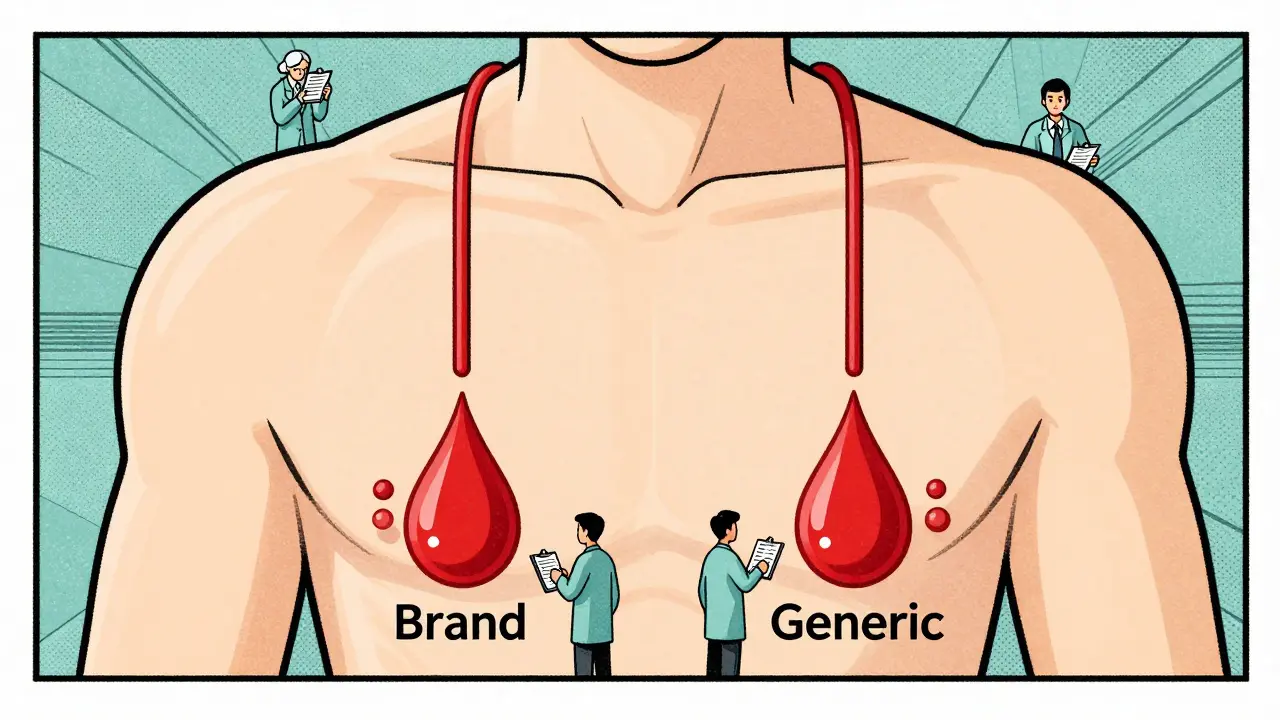
How do they prove that? Through blood tests. Researchers measure how much of the drug enters your bloodstream (AUC) and how fast it peaks (Cmax). The FDA requires these numbers to fall within 80% to 125% of the brand’s values. That’s not a wide gap. It’s tight enough to ensure your body reacts the same way.
That’s why 90% of prescriptions in the U.S. are for generics. They save patients and the system an average of 80-85% per drug. In 2023, generics made up 90.7% of all prescriptions but only 18.3% of total drug spending. That’s not magic - it’s science.
What does the real-world data say?
Let’s look at hard numbers. A 2020 study in Nature Scientific Reports tracked over 1.5 million Austrians on generic vs. brand medications between 2007 and 2012. The results? Generics were linked to fewer deaths in 10 out of 17 drugs studied. For heart attacks and strokes combined, patients on generics had 40% fewer major events. That’s not a fluke. The researchers adjusted for age, income, and other factors - and the trend held.
Another study from the FDA’s own adverse event database (2018-2022) looked at 15 common drugs. For every million prescriptions, generics had 12.7 reports of side effects. Brands had 13.2. That’s statistically the same.
Consumer Reports’ 2022 survey of 10,000 U.S. adults found 89% reported no difference between generic and brand drugs. Most people - the vast majority - can’t tell the difference.
But what about the cases where it didn’t work?
Here’s where it gets messy. Not every drug is created equal. Some medicines have what’s called a narrow therapeutic index. That means the difference between a dose that works and one that’s dangerous is tiny. For these drugs, even small changes in how the body absorbs the drug can matter.
Examples include:
- Levothyroxine (for thyroid disease)
- Warfarin (a blood thinner)
- Phenytoin and carbamazepine (for seizures)
There are real stories. One Reddit user switched from Synthroid to generic levothyroxine and saw their TSH level jump from 1.2 to 8.7 - a sign their thyroid wasn’t getting enough hormone. Another patient on generic warfarin had a dangerous clot after switching, despite being told the dose was "the same."
A 2017 Canadian study of over 136,000 seniors found a spike in hospital visits for blood pressure drugs like losartan and valsartan in the month after generics hit the market. The increase? 8% to 14%. It wasn’t massive - but it was real.
Why does this happen? It’s not about the active ingredient. It’s about the rest. Generics can use different fillers, binders, and coatings. These "inactive ingredients" can affect how fast the pill breaks down in your stomach. For most drugs, that doesn’t matter. For a thyroid pill? It can.
What do experts really think?
Dr. Aaron Kesselheim, lead author of the 2020 study, says generics are "at least similar, and in some cases superior" to brands. He points out that generic manufacturers now compete on quality - not just price. Many are owned by the same big pharma companies that make the originals.
But experts also warn. The American College of Clinical Pharmacy says while most generics are fine, "theoretical concerns exist" - especially with drugs where tiny changes can cause big problems. The FDA agrees. Their official stance: "Generic drugs work the same as brand-name drugs." But they also say: "For some patients, switching may require monitoring."
Harvard Medical School’s Dr. Niteesh Choudhry puts it simply: "The existing data are reassuring." But he also notes that the Canadian study on blood pressure drugs "raised important questions."
What should you do if you’re on a generic?
If you’re taking a generic drug and feel fine - keep taking it. Don’t switch back to the brand unless your doctor says so. The odds are overwhelmingly in your favor.
But if you’re on one of those narrow therapeutic index drugs - levothyroxine, warfarin, seizure meds - here’s what to do:
- Don’t switch back and forth. If you started on a brand, stay on it. If you started on a generic, stay on that one. Consistency matters more than the name.
- Ask your pharmacist. Ask if your generic is from the same manufacturer each time. Some pharmacies rotate suppliers. That’s fine for most drugs - but not for thyroid or blood thinners.
- Get your levels checked. If you’re on levothyroxine, ask for a TSH test 6-8 weeks after switching. For warfarin, check your INR. These tests tell you if the drug is working - not what the label says.
- Speak up. If you feel worse after switching - fatigue, dizziness, palpitations - tell your doctor. Don’t assume it’s "all in your head."

Why do some doctors still hesitate?
A 2021 study found only 43% of physicians regularly check the FDA’s Orange Book - the official list of approved generics and their equivalence ratings. Many don’t know which generics are AB-rated (therapeutically equivalent) and which aren’t.
Pharmacists can legally substitute generics unless the doctor writes "Dispense as Written." But if the doctor doesn’t know the difference, they might not block a switch that could be risky.
That’s why patient advocacy matters. If you’re on a critical drug, ask: "Is this generic approved as equivalent?" And if your doctor says "yes," ask: "Can I get a copy of the Orange Book rating?"
What’s changing in 2026?
The FDA is tightening oversight. In 2022, they approved 1,107 generics - up 12% from the year before. But they’re also cracking down on quality. In 2022, 17 import alerts were issued for generic drug makers due to contamination or manufacturing issues.
The FDA’s new 2023 guidance focuses on complex generics - inhalers, topical creams, injectables - where traditional blood tests aren’t enough. These drugs may need new testing methods to prove they work the same.
And with over $250 billion in brand-name drugs set to lose patent protection by 2028, we’ll see even more generics hit the market. That means more competition - and more pressure on manufacturers to deliver consistent quality.
The bottom line
Generic drugs are safe for 9 out of 10 people. The science is clear. The savings are real. For most medications - antibiotics, statins, blood pressure pills - you’re not losing anything by choosing the generic.
But for thyroid, blood thinners, and seizure drugs? Pay attention. Stick with one version. Monitor your numbers. Don’t assume "same dose = same effect."
The system works. But it works best when you’re informed.
Are generic drugs less effective than brand-name drugs?
For most drugs, no. Generic drugs are required by the FDA to have the same active ingredient, strength, and bioavailability as brand-name versions. Studies tracking millions of patients show no meaningful difference in effectiveness or safety for the vast majority of medications. However, for drugs with a narrow therapeutic index - like levothyroxine, warfarin, or certain seizure medications - small differences in absorption can matter. In these cases, staying on the same formulation - brand or generic - is recommended.
Why do some people say generics don’t work for them?
Some patients report feeling worse after switching to a generic. This can happen due to differences in inactive ingredients - fillers, dyes, coatings - that affect how quickly the drug dissolves in the body. For most drugs, this doesn’t matter. But for thyroid, blood thinners, or epilepsy meds, even a 10% change in absorption can throw off your balance. Psychological factors also play a role: if you believe generics are inferior, your body might react as if they are. Always talk to your doctor if you notice changes after switching.
Can I switch between different generic brands?
For most medications, yes - generics from different manufacturers are equally safe. But for drugs with a narrow therapeutic index - such as levothyroxine, warfarin, or phenytoin - switching between generics can cause instability. The FDA considers all AB-rated generics equivalent, but real-world experience shows some patients are sensitive to changes in fillers or dissolution rates. If you’re on one of these drugs, it’s best to stick with one manufacturer unless your doctor advises otherwise.
How do I know if my generic is FDA-approved?
All FDA-approved generics are listed in the Orange Book, which you can search online. Look for the "AB" rating - that means the generic is therapeutically equivalent to the brand. Your pharmacist can also tell you if the generic you’re getting is AB-rated. If your prescription says "Dispense as Written," your doctor has asked the pharmacy not to substitute - that’s often done for sensitive medications.
Do generic drugs have more side effects?
No - overall, generic drugs have similar side effect rates to brand-name drugs. The FDA’s adverse event database (FAERS) shows nearly identical reporting rates per million prescriptions. However, a small percentage of patients - especially those on thyroid, seizure, or blood-thinning drugs - report new or worsening side effects after switching. This is often due to differences in inactive ingredients or absorption, not the active drug itself. If you experience unusual symptoms after switching, contact your doctor.
