When you take a tricyclic antidepressant like amitriptyline or nortriptyline for depression or chronic pain, you might not realize you’re also loading your body with a hidden risk - one that can blur the line between normal aging and early dementia, or trigger a dangerous heart rhythm without warning. These drugs work by boosting serotonin and norepinephrine, yes - but they also block acetylcholine, a key brain chemical that controls memory, attention, and even your heartbeat. This blocking effect is called anticholinergic burden, and it’s not just a side effect. It’s a measurable, cumulative threat that grows with every pill you take, especially if you’re over 50.
What Is Anticholinergic Burden, Really?
Anticholinergic burden isn’t a vague warning. It’s a score. Clinicians use tools like the Anticholinergic Cognitive Burden (ACB) Scale to rate how strongly a drug blocks acetylcholine. Scores range from 1 (possible effect) to 3 (definite, high effect). Tricyclic antidepressants? They all score a 3. That’s the highest possible. Amitriptyline, doxepin, clomipramine - they’re all in the same dangerous category as over-the-counter sleep aids like diphenhydramine and bladder meds like oxybutynin. That’s not a coincidence. It’s a red flag.Here’s what that means in practice: if you’re taking one TCA, your ACB score is already 3. If you’re also taking an antihistamine for allergies or a sleep aid at night, your score jumps to 5 or higher. Research shows that once your total ACB score hits 3 or more, your risk of developing dementia over the next 7 years increases by 54%. And here’s the chilling part - that risk doesn’t disappear when you stop the drug. Some cognitive damage may be permanent.
Why TCAs Are Worse Than Other Antidepressants
Modern antidepressants like sertraline, escitalopram, or venlafaxine barely register on the ACB scale. Most have scores of 0 or 1. They don’t mess with acetylcholine the way TCAs do. That’s why guidelines from NICE and the Beers Criteria now say: avoid TCAs in adults over 65 unless every other option has failed.It’s not that TCAs don’t work. They do - especially for treatment-resistant depression or neuropathic pain. But their benefits are narrow. Their risks are wide. A 2023 study in Age and Ageing found that older adults who switched from TCAs to low-anticholinergic alternatives saw their MMSE cognitive scores improve by an average of 2.7 points within a year. That’s not a small gain - it’s the difference between forgetting where you put your keys and forgetting how to get home.
And it’s not just the brain. The heart is equally at risk.
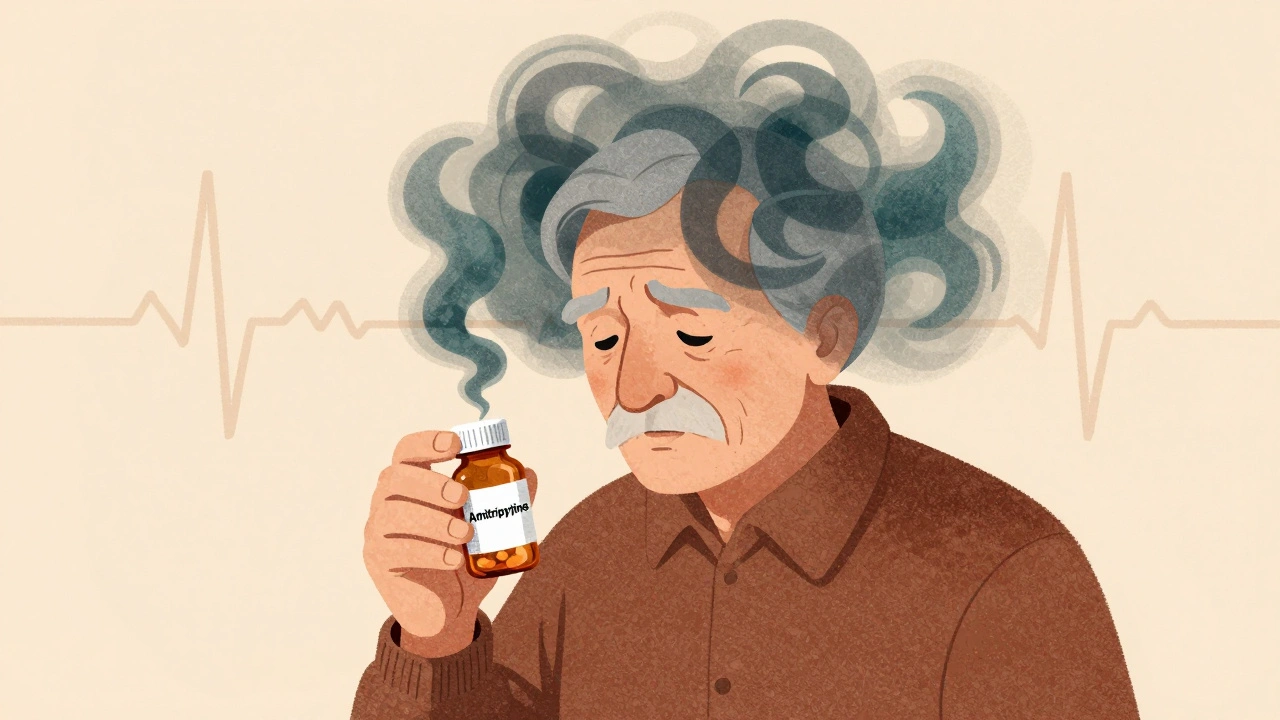
The Hidden Heart Danger
TCAs don’t just slow your thinking - they can slow or scramble your heartbeat. They act like Class 1A antiarrhythmics, but without the safety controls. At therapeutic doses, amitriptyline can prolong the QRS complex on an ECG by 10-25%. In overdose, that jumps to 50%. That’s not theoretical. Emergency rooms see this regularly. Patients on TCAs show up with palpitations, dizziness, or fainting - only to find their QT interval is dangerously long.Compared to SSRIs, TCAs carry about three times the risk of arrhythmias. Amitriptyline specifically is linked to 2.8 times higher risk of QT prolongation than sertraline. For someone with existing heart disease, high blood pressure, or electrolyte imbalances, this isn’t just risky - it’s life-threatening. A 2022 report from the Mended Hearts patient forum described a 71-year-old man who ended up in the ER after three weeks on amitriptyline. His ECG showed a prolonged QT interval. He had no prior heart history. His doctor hadn’t checked his ECG before prescribing.
What Patients Actually Experience
Real people don’t talk about ACB scores. They talk about dry mouth so bad they need artificial saliva every night. Constipation that requires daily laxatives. Blurry vision that makes reading impossible. Memory lapses they blame on aging - until they realize they’ve forgotten their grandchild’s name three times this week.A 2022 survey by the National Council on Aging found 68% of patients over 65 on TCAs had at least two major anticholinergic side effects. One in three said the cognitive symptoms were bad enough to consider quitting. On Reddit’s r/psychiatry, clinicians share stories of patients diagnosed with early dementia - only to have their symptoms vanish after stopping the TCA. One doctor wrote: “I had a 68-year-old woman labeled with mild cognitive impairment. She was on amitriptyline for back pain. We stopped it. Three months later, she was back to her normal self. No dementia. Just drug-induced fog.”
What Should You Do?
If you’re taking a TCA, here’s what matters:- Ask for your total ACB score. Don’t assume your doctor knows - ask them to calculate it. Include every pill, even OTC sleep aids or allergy meds.
- If your score is 3 or higher, ask if there’s a safer alternative. SNRIs like duloxetine or venlafaxine work nearly as well for pain and depression with almost no anticholinergic effect.
- Never stop abruptly. TCAs can cause withdrawal symptoms like nausea, insomnia, and mood swings. Tapering over 4-8 weeks is essential.
- Get an ECG before starting and after 4-6 weeks. Look for QRS widening or QT prolongation. If you’re over 60, this isn’t optional.
- If you’re on multiple medications, ask for a full medication review. Many people don’t realize their daily Benadryl or NyQuil adds to the burden.
Deprescribing TCAs isn’t a failure - it’s smart medicine. NHS Somerset’s programs show that 78% of older patients successfully reduced their anticholinergic burden, and 63% saw measurable cognitive improvements within six months. That’s not a miracle. It’s just removing a toxin that was never meant to be long-term.

The Bigger Picture
Prescribing TCAs has dropped sharply in the U.S. - from 15% of all antidepressant prescriptions in 2000 to just 4.7% in 2020. Why? Because the data is clear. The risks outweigh the benefits for most people. Newer antidepressants approved since 2010 have almost zero anticholinergic activity. Why stick with a 1950s drug when safer, just-as-effective options exist?Some argue TCAs are still useful for treatment-resistant cases. Maybe. But even then, they should be used short-term, with close monitoring, and only after other options are exhausted. The idea that “it’s worked for years” isn’t enough. If your memory’s fading or your heart’s skipping beats, it’s not working - it’s harming.
The future is automated. UK hospitals are now piloting AI systems that flag high ACB scores during e-prescribing. If your doctor tries to write a prescription for amitriptyline and you’re on three other anticholinergics, the system will pop up a warning. That’s not sci-fi - it’s already happening. The medical world is finally catching up to what the science has said for years.
Final Thought
Anticholinergic burden isn’t a footnote. It’s the main story. TCAs are powerful tools - but they’re also blunt instruments. In a world where we have precision tools for depression and pain, why settle for something that clouds your mind and strains your heart? If you’re on a TCA, don’t wait for symptoms to get worse. Ask for a review. Ask for a score. Ask for a plan. Your brain and your heart will thank you.Can tricyclic antidepressants cause dementia?
Yes, long-term use of tricyclic antidepressants (TCAs) is strongly linked to an increased risk of dementia. A landmark study tracking over 3,400 adults over 65 for seven years found that those taking medications with high anticholinergic burden - including TCAs - had a 54% higher risk of developing dementia. The effect may be irreversible, even after stopping the drug. This isn’t just correlation; it’s a direct result of acetylcholine blockade in the brain, which disrupts memory and learning pathways.
Is amitriptyline safe for older adults?
No, amitriptyline is not considered safe for older adults as a first-line treatment. It has the highest possible anticholinergic burden score (ACB=3) and significantly increases risks of cognitive decline, falls, urinary retention, and dangerous heart rhythm changes. Guidelines from NICE and the Beers Criteria recommend avoiding it in people over 65 unless all other options have failed and the benefits clearly outweigh the risks. Even then, it should be used at the lowest possible dose for the shortest time.
What are safer alternatives to tricyclic antidepressants?
Safer alternatives include SSRIs like sertraline or escitalopram, and SNRIs like duloxetine or venlafaxine, which have ACB scores of 0 or 1 - meaning minimal anticholinergic effects. For neuropathic pain, duloxetine is often equally effective as amitriptyline but without the cognitive or cardiac risks. Non-drug options like cognitive behavioral therapy (CBT), physical therapy, or mindfulness-based stress reduction can also be effective, especially when combined with medication.
How do I know if I’m taking too many anticholinergic drugs?
Add up the ACB scores of all your medications - including over-the-counter ones like diphenhydramine (Benadryl), chlorphenamine (Piriton), or oxybutynin. If your total score is 3 or higher, you’re at increased risk. Common signs include dry mouth, constipation, blurred vision, confusion, memory lapses, or trouble urinating. If you’re over 50 and taking multiple medications, ask your doctor to run a full anticholinergic burden assessment using the ACB scale. Many electronic health systems now flag high-risk combinations automatically.
Can stopping a tricyclic antidepressant improve cognitive function?
Yes. In clinical programs that carefully taper patients off TCAs, 63% of older adults showed measurable cognitive improvement within six months. Memory, attention, and processing speed often get better - sometimes dramatically. One study showed average Mini-Mental State Examination (MMSE) scores rising by 2.7 points after switching to low-anticholinergic alternatives. This isn’t temporary; it’s the brain recovering from chemical suppression. If you’ve been on a TCA for years and feel mentally foggy, stopping it - under medical supervision - might be the best thing you can do for your brain.
Do all tricyclic antidepressants have the same risk?
All TCAs have an ACB score of 3 - meaning they’re all classified as highly anticholinergic. However, nortriptyline is slightly less potent in blocking acetylcholine than amitriptyline, so some clinicians consider it marginally safer. But the difference is small. Both can cause significant cognitive and cardiac side effects. Neither should be used casually, especially in older adults. The key isn’t choosing the “least bad” TCA - it’s finding a non-anticholinergic alternative.
Should I get an ECG before starting a tricyclic antidepressant?
Absolutely. TCAs can prolong the QT interval and widen the QRS complex on an ECG, increasing the risk of life-threatening arrhythmias. This risk is higher in people over 60, those with heart disease, or those taking other QT-prolonging drugs. A baseline ECG before starting, and another after 4-6 weeks, is a standard safety step that many doctors still skip. Don’t assume you’re fine - ask for it. It takes five minutes and could save your life.
Michael Bene
December 3, 2025 AT 23:37
Let me tell you something - I’ve been on amitriptyline for seven years for my back pain. Last year I started forgetting my wife’s birthday. Not just the date - I forgot who she was for like 40 seconds. I thought she was a neighbor. Then I read this post. Got off the drug. Three months later, I remembered how to spell ‘spaghetti’ again. This isn’t medicine. It’s chemical lobotomy with a side of dry mouth.
Brian Perry
December 4, 2025 AT 14:47
bro i was on nortriptyline and my brain felt like it was wrapped in saran wrap dipped in honey… then i stopped and now i can read a book without falling asleep after 3 sentences. also my dick works better. just saying.
Ethan McIvor
December 4, 2025 AT 18:20
It’s funny how we treat the brain like a machine you can tweak with pills, then act surprised when it starts glitching. We’re not just blocking acetylcholine - we’re silencing the voice that remembers your mother’s laugh, the smell of rain on pavement, the name of your first pet. These drugs don’t just cause dementia… they steal the moments that make life worth remembering. And we call it treatment?
Maybe we’re not treating depression. Maybe we’re just numbing the pain of being human.
Mindy Bilotta
December 5, 2025 AT 14:55
my 72-year-old mom was on amitriptyline for 12 years. she kept saying she was just ‘getting forgetful.’ we thought it was aging. then her new dr checked her meds - she was on benadryl, oxybutynin, AND amitriptyline. ACB score of 9. we tapered her off. six months later? She started knitting again. Remembered her childhood dog’s name. Said she felt like she ‘woke up.’
if you’re on a TCA and feel foggy - don’t wait. ask for a review. your brain isn’t broken. it’s just drugged.
Chloe Madison
December 5, 2025 AT 14:55
YOU ARE NOT ALONE. I know how scary it feels to realize your memory isn’t fading - it’s being poisoned. But here’s the good news: you can take back your mind. It’s not too late. Talk to your doctor. Get your ACB score. Swap that TCA for an SSRI or SNRI. You’re not weak for wanting to feel clear-headed. You’re brave for asking. Your brain deserves better than a 1950s relic. You’ve got this. 💪🧠
Vincent Soldja
December 7, 2025 AT 02:41
TCAs are dangerous in elderly patients. Guidelines clearly state this. ECG monitoring is mandatory. If your doctor isn’t doing it they are negligent. End of story.
Makenzie Keely
December 8, 2025 AT 00:29
As someone who works in geriatric pharmacy, I see this every single week. A patient comes in with ‘memory issues’ - turns out they’re on amitriptyline, diphenhydramine, oxybutynin, and chlorpheniramine. Total ACB score: 11. They’re not ‘demented’ - they’re pharmacologically sedated. We switch them, and within weeks? They’re laughing again. Talking to their grandkids. Remembering where they put their glasses. It’s not magic. It’s just removing the poison.
And yes - the AI flags are already live in 12 UK hospitals. We’re not lagging behind. We’re just slow to admit it.
Joykrishna Banerjee
December 8, 2025 AT 16:04
Oh please. You’re all overreacting to a 1950s pharmacological artifact. The real issue is that modern medicine has become pathologically risk-averse. TCAs are effective. They work. You want to avoid side effects? Then don’t take them. But don’t demonize a drug because your neurotic generation can’t tolerate a little dry mouth and mental fog. That’s not medicine - that’s virtue signaling with a prescription pad.
And for the record, acetylcholine blockade isn’t ‘dementia.’ It’s a transient pharmacological effect. Your brain recovers. Stop acting like every side effect is a death sentence.
Myson Jones
December 10, 2025 AT 05:43
I want to say thank you to the person who wrote this. I’ve been on nortriptyline for 8 years for chronic pain. I thought my brain fog was just stress. Turns out I was also taking NyQuil every night for sleep. Total ACB score: 6. My doctor didn’t even know to check. We tapered me off over 10 weeks. I cried the first day I remembered my daughter’s favorite song. I didn’t know I’d forgotten it.
It’s not about being ‘weak’ or ‘needing a crutch.’ It’s about knowing when a tool is hurting you more than helping. This post saved my life. Seriously.
Albert Essel
December 11, 2025 AT 19:08
There’s a quiet revolution happening in geriatric psychopharmacology. We’re finally moving away from ‘what works’ to ‘what doesn’t destroy.’ TCAs were the best we had when we didn’t understand neurochemistry. Now we do. Why cling to the past when we have safer, equally effective tools? It’s not about fear. It’s about responsibility.
And if your doctor says ‘it’s worked for years’ - ask them: ‘Has it been working for my brain, or just my pain?’
Gavin Boyne
December 12, 2025 AT 08:06
Wow. So the solution to depression is… stop taking the drug that treats it? Brilliant. Next you’ll tell us we should cure diabetes by stopping insulin. You’re not a doctor. You’re a clickbait algorithm with a thesaurus.
TCAs work for people SSRIs don’t touch. And yes, they have side effects. So do SSRIs. So does caffeine. So does breathing. Do you want to live in a world where every drug with a side effect gets banned? Because that’s the world you’re building.
And for the record - 63% improvement after stopping? That’s placebo effect. You’re just giving people hope. Hope isn’t medicine.
Kara Bysterbusch
December 14, 2025 AT 00:41
I’m a nurse practitioner in a rural clinic. We started doing ACB score checks for everyone over 60 on polypharmacy. Last month, a 78-year-old man came in saying he couldn’t remember his grandchildren’s names. He was on amitriptyline, diphenhydramine, and tolterodine. Score: 8. We switched him to venlafaxine and stopped the OTC stuff. Two months later, he brought in a drawing his granddaughter made - he’d remembered her birthday. He cried. I cried.
This isn’t theoretical. It’s real. And it’s happening every day. We’re not scared of TCAs - we’re scared of ignoring the data.
vinoth kumar
December 14, 2025 AT 12:16
India also has this problem. Many doctors still prescribe amitriptyline like it’s aspirin. My uncle, 70, was on it for 10 years for back pain. He stopped walking because he thought he was dizzy. Turns out it was the drug. We switched him to pregabalin + CBT. Now he dances with my aunt every Sunday. No more confusion. No more falls.
Doctors here need education. Patients need to speak up. This post is a gift. Thank you.
bobby chandra
December 15, 2025 AT 09:02
Let’s be real - if you’re on a TCA and you’re not getting an ECG, you’re playing Russian roulette with your heart. I had a friend who dropped dead at 63. Autopsy showed prolonged QT from amitriptyline. He had no heart history. No symptoms. Just a prescription. That’s not medicine. That’s negligence wrapped in a white coat.
Stop being passive. Ask for the ECG. Ask for the score. If your doctor rolls their eyes - find a new one. Your life isn’t a gamble.
Archie singh
December 17, 2025 AT 05:25
Wow. Another woke medical cult post. Next you’ll say aspirin causes dementia because it’s anti-inflammatory. Pathetic. You people are scared of side effects. That’s why America is full of zombies on SSRIs who can’t feel joy, but at least they’re ‘safe.’
TCAs work. They’re cheap. They’re effective. Stop trying to make medicine a purity test. You don’t get to decide what’s ‘safe’ for everyone. Only a doctor who knows the patient does.