Penicillin Allergy: Symptoms, Alternatives, and What to Do If You're Misdiagnosed
When someone says they have a penicillin allergy, an immune system reaction to penicillin antibiotics that can range from mild rash to life-threatening anaphylaxis. Also known as beta-lactam allergy, it’s one of the most commonly reported drug allergies in the U.S. But here’s the catch: more than 90% of people who think they’re allergic to penicillin aren’t. Many outgrew it. Others had a rash as a kid that wasn’t a true allergy—maybe it was a virus, or a side effect, not an immune response. Yet they avoid penicillin for life, even when it’s the best, safest, or cheapest option.
This matters because avoiding penicillin often means switching to broader-spectrum antibiotics like vancomycin or clindamycin, which can lead to more side effects, higher costs, and even antibiotic resistance. A true penicillin allergy, an IgE-mediated reaction triggered by the drug’s structure usually shows up within an hour: hives, swelling, trouble breathing, or low blood pressure. A delayed rash—like the one some get with amoxicillin, a common penicillin-type antibiotic often prescribed for ear infections or sinusitis—is rarely dangerous. It’s more likely a viral rash, especially in kids with mono or Epstein-Barr. And here’s the kicker: if you’ve never had a severe reaction, you might not need to avoid it at all.
That’s why drug allergy testing, a simple skin test followed by an oral challenge under medical supervision is so important. It’s safe, fast, and covered by most insurance. If you were told you’re allergic to penicillin as a child and haven’t taken it since, getting tested could open up better treatment options for you or your kids. Even if you had a reaction, it doesn’t mean you’re allergic forever. Allergies fade over time.
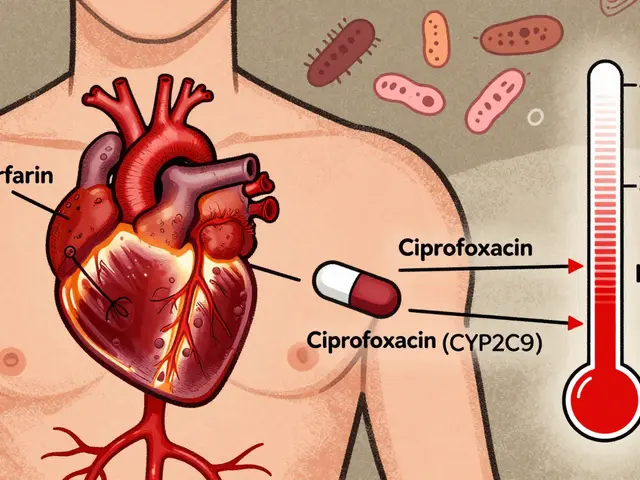
And if you do have a confirmed allergy, you’re not stuck with limited choices. There are plenty of penicillin alternatives, antibiotics like azithromycin, ciprofloxacin, or sulfamethoxazole that work just as well for common infections. But the goal isn’t just to swap one drug for another—it’s to use the right one, the safest one, and avoid unnecessary risks.
In the posts below, you’ll find real-world stories and science-backed advice about what penicillin allergy really means, how to tell if you’re truly allergic, what symptoms to watch for, and which antibiotics you can safely take instead. Some posts dive into how hospitals handle these cases. Others show how mislabeling leads to worse outcomes. You’ll see how testing changes lives—and why so many people are needlessly avoiding a drug that could save them time, money, and complications.