Steroid-PPI Risk Calculator
Calculate Your PPI Need
Based on evidence from major medical guidelines, determine if you need PPI prophylaxis when taking corticosteroids.
Results
Recommendation
Low RiskWhy This Recommendation?
For years, doctors have assumed that taking corticosteroids like prednisone puts you at high risk for stomach ulcers. But the truth is more complicated than that. If you're on steroids alone - no NSAIDs, no history of ulcers, not in the hospital - your risk of developing a gastric ulcer is extremely low. In fact, studies show it’s around 0.4% to 1.8%. That’s less than 2 in 100 people. Yet, most patients on steroids are still handed a proton pump inhibitor (PPI) like omeprazole as a matter of routine. Why? Because old habits die hard.
What’s Really Going On With Steroids and Stomach Ulcers?
Corticosteroids don’t directly cause ulcers the way NSAIDs do. NSAIDs block protective prostaglandins in the stomach lining, leaving it exposed to acid. Steroids? They work differently. They suppress inflammation, slow tissue repair, and can mask pain. So if an ulcer forms - maybe from another cause - steroids might keep you from feeling the warning signs until it’s too late. That’s why complications like bleeding or perforation can sneak up.
A 2014 review in BMJ Open looked at over a million patients. It found that for people taking steroids in outpatient settings - meaning, most of us - there was no significant increase in GI bleeding. But for hospitalized patients? Risk jumped by 43%. Why? Because they’re sicker, often on multiple drugs, and their bodies are under more stress. The real danger isn’t the steroid alone. It’s the combo.
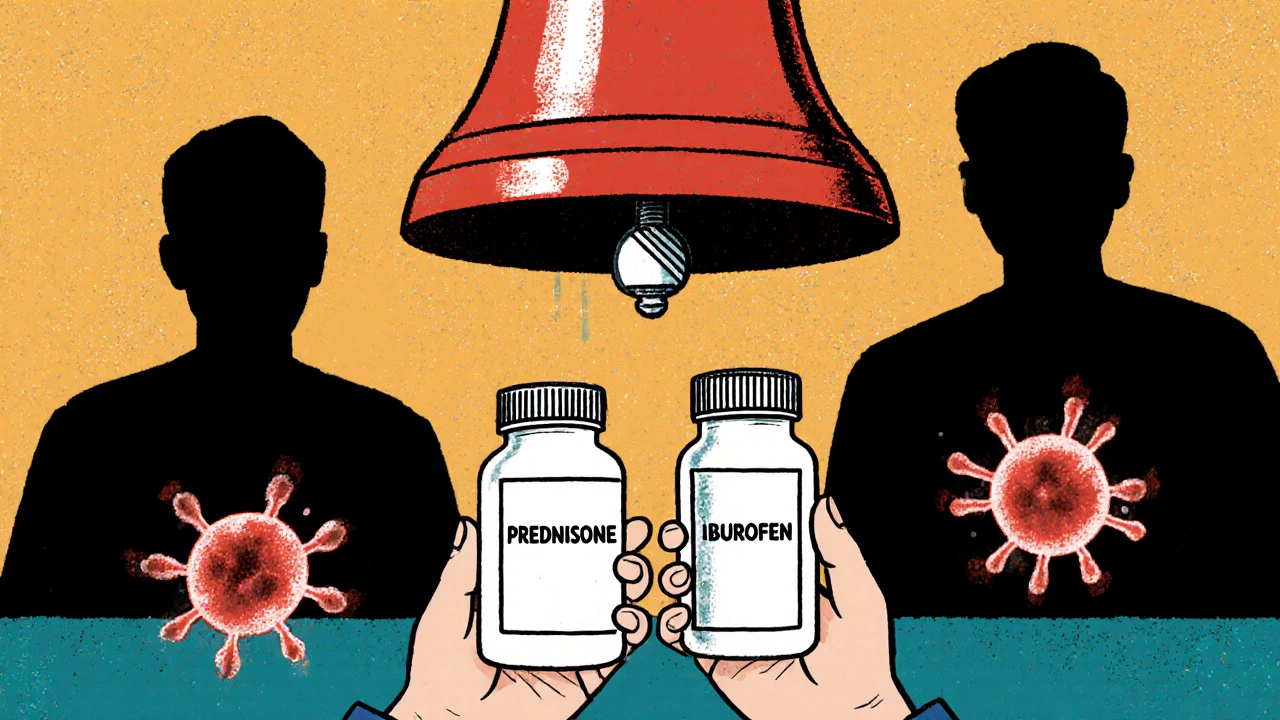
The Big Red Flag: NSAIDs and Steroids Together
If you’re taking both corticosteroids and NSAIDs - like ibuprofen, naproxen, or even low-dose aspirin - your risk of a serious GI event goes up dramatically. One study of Medicaid patients showed a 4.4-fold increase in ulcer complications when these drugs were used together. That’s not a small bump. That’s a red alert.
Here’s the hard truth: if you’re on both, you need protection. PPIs are the go-to. Misoprostol works too, but it causes cramping and diarrhea in many people, so it’s not first-line. The evidence here is solid. Don’t skip this step. If you’re on steroids for a flare-up of rheumatoid arthritis or lupus and you’re also taking ibuprofen for joint pain, you’re playing with fire. Talk to your doctor about switching to acetaminophen or finding another pain control plan.
Why So Many People Get Unnecessary PPIs
A 2022 survey of 347 hospitalists found that nearly 80% routinely prescribed PPIs to patients on high-dose steroids - even when they weren’t taking NSAIDs. But here’s the kicker: 63% of those doctors admitted they didn’t have strong evidence to support it. So why do it? Fear. Tradition. And the belief that it’s "better safe than sorry."
But "better safe" isn’t always better. PPIs aren’t harmless. Long-term use links to vitamin B12 deficiency, low magnesium, increased risk of C. diff infections, and even bone fractures. Taking a PPI when you don’t need it is like using a sledgehammer to crack a nut - you might fix the problem, but you create new ones.
At Johns Hopkins, a quality improvement project stopped routine PPIs for steroid-only patients. Over 12 months, PPI use dropped by 42.7%. And guess what? No rise in ulcers or bleeding. At the University of Wisconsin, they cut inappropriate PPI prescriptions by 35% after introducing a simple protocol: only give PPIs if you’re also on NSAIDs, have a past ulcer, or are hospitalized.
Who Actually Needs Protection?
Not everyone. But some people definitely do. Here’s who should get a PPI or other gastroprotective therapy:
- You’re taking both corticosteroids and NSAIDs
- You have a history of peptic ulcer disease or GI bleeding
- You’re on anticoagulants like warfarin or apixaban
- You’re in the hospital, especially if you’re critically ill
- You’re over 65 and on high-dose steroids (>20mg prednisone daily)
If none of those apply to you, you probably don’t need a PPI. Ask your doctor. If they say "it’s standard," ask them to show you the evidence. The American College of Gastroenterology doesn’t recommend routine prophylaxis for steroid monotherapy. Neither does the American Gastroenterological Association - and they’re reviewing it again in 2025.
Monitoring: What to Watch For
Even if you’re not on a PPI, you still need to monitor. Ulcers don’t always scream. Sometimes they whisper - and by the time you hear it, it’s too late.
Pay attention to these red flags:
- Black, tarry stools (melena)
- Vomiting blood or material that looks like coffee grounds
- Unexplained fatigue or dizziness (signs of anemia from slow bleeding)
- Persistent upper abdominal pain that doesn’t go away with antacids
- Loss of appetite or unexplained weight loss
If you notice any of these, get checked. Don’t wait. Endoscopy is the gold standard for diagnosis - and it’s a quick, safe procedure. Don’t let fear of the test stop you. It’s better than a surprise bleed.
Also, monitor your blood sugar. Steroids cause insulin resistance. Post-meal spikes are more common than fasting highs. If you’re prediabetic or diabetic, your glucose levels may climb even on low doses. Check your levels regularly. Adjust your diet. Talk to your doctor about whether your diabetes meds need tweaking.
What About H. pylori?
Helicobacter pylori is the #1 cause of peptic ulcers worldwide. Steroids don’t cause it - but if you have it, they can make things worse. If you’ve had an ulcer before, or if you’re from a region with high H. pylori rates (like parts of Asia, Eastern Europe, or Latin America), ask your doctor about testing. A simple breath test or stool antigen test can detect it. If positive, treatment with antibiotics and a PPI clears it in most cases - and removes a major risk factor.
The Bottom Line: No One-Size-Fits-All
The old rule - "steroids mean PPIs" - is outdated. It’s not evidence-based. It’s not cost-effective. And it’s potentially harmful.
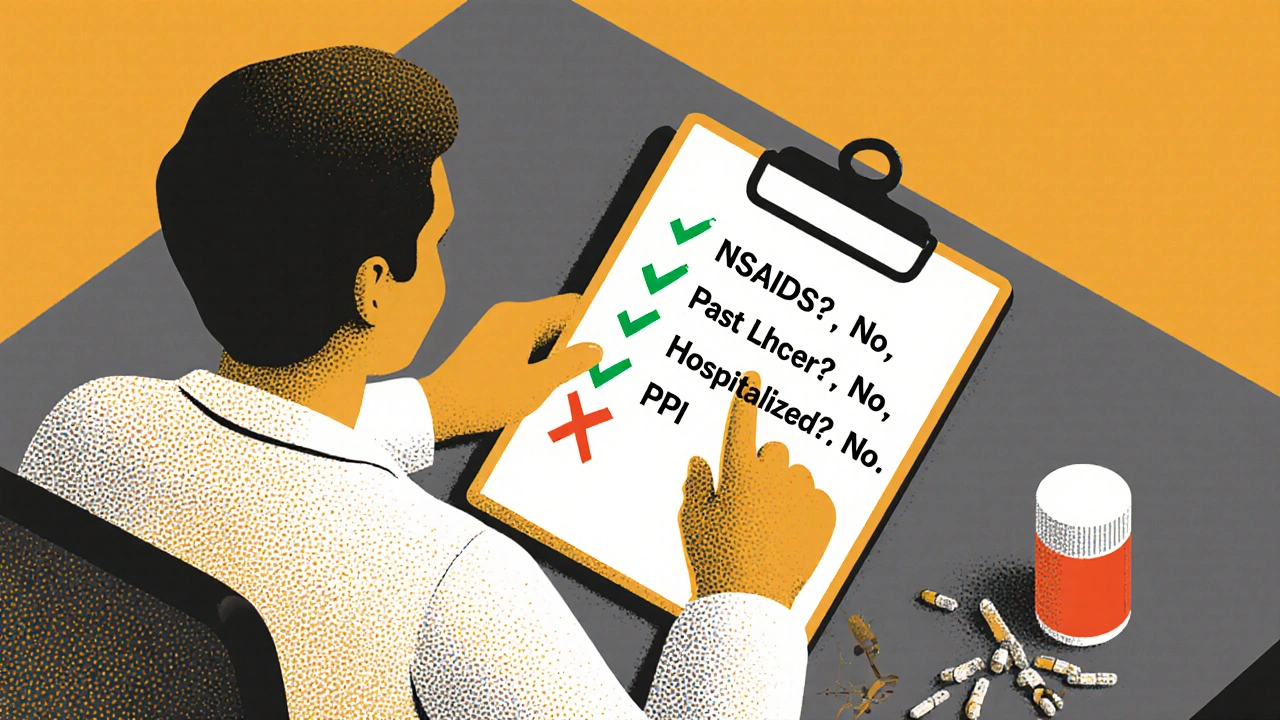
Here’s what you should do instead:
- Ask your doctor: "Am I taking NSAIDs?" If yes, you need a PPI.
- Do you have a history of ulcers or GI bleeding? If yes, you need a PPI.
- Are you in the hospital? If yes, you likely need a PPI.
- Are you on high-dose steroids (>20mg prednisone) and over 65? Consider a PPI, but discuss the risks.
- If none of the above apply? You probably don’t need a PPI. Say no - politely - and ask for the evidence.
And if you’re already on a PPI for steroids alone? Don’t stop cold turkey. Talk to your doctor. They may be able to taper it off safely - especially if you’ve been on it for months or years.
The goal isn’t to avoid all medications. It’s to take only what you need. Steroids save lives. But unnecessary PPIs? They just add clutter to your pillbox - and risk to your health.
Do corticosteroids cause stomach ulcers on their own?
No, corticosteroids alone rarely cause ulcers. Studies show the risk is very low - between 0.4% and 1.8% - in people not taking NSAIDs or with no prior ulcer history. The real danger comes when steroids are combined with NSAIDs, anticoagulants, or in hospitalized patients.
Should everyone on steroids take a PPI?
No. Routine PPI use for steroid monotherapy is not supported by evidence. Major medical groups, including the American College of Gastroenterology, do not recommend it. PPIs should only be used if you have other risk factors like NSAID use, past ulcers, or hospitalization.
What are the risks of taking PPIs long-term?
Long-term PPI use can lead to vitamin B12 deficiency, low magnesium levels, increased risk of C. diff infection, and higher chances of bone fractures. It may also mask symptoms of stomach cancer. Taking PPIs when you don’t need them exposes you to these risks without benefit.
Can I stop my PPI if I’m only on steroids?
Yes - but don’t stop abruptly. Talk to your doctor. If you’re not on NSAIDs, have no history of ulcers, and aren’t hospitalized, you likely don’t need it. Your doctor can help you taper off safely, especially if you’ve been on it for months.
How do I know if I have a steroid-related ulcer?
Look for black or tarry stools, vomiting blood, unexplained fatigue, persistent upper abdominal pain, or sudden weight loss. These are alarm symptoms. Don’t wait - get an endoscopy if they occur. Steroids can mask pain, so symptoms may appear late.
Is H. pylori testing important if I’m on steroids?
Yes, especially if you’ve had a prior ulcer, are over 50, or come from a region with high H. pylori rates. The bacteria is the leading cause of ulcers. Steroids won’t cause it, but they can worsen damage if it’s present. A simple stool or breath test can detect it - and treatment is very effective.

Yash Hemrajani
November 29, 2025 AT 13:06
So let me get this straight - we’re giving PPIs to healthy people on steroids like they’re candy at a parade, just because someone in 1997 thought it was a good idea? 🤦♂️ Meanwhile, the real problem - NSAID + steroid combos - is getting ignored while we’re busy turning every outpatient into a proton pump addict. The medical industrial complex runs on habit, not science. Thanks for calling it out.
Pawittar Singh
November 29, 2025 AT 17:22
Y’all need to stop treating PPIs like vitamins 😊 This isn’t just about saving money - it’s about protecting your gut long-term. I’ve seen patients on PPIs for 10+ years with B12 levels so low they were practically ghosts. If you’re not on NSAIDs or in the hospital, you don’t need it. Ask your doc. Show them this post. You got this 💪
Josh Evans
November 29, 2025 AT 22:03
This is exactly why I stopped taking my omeprazole last year. I was on prednisone for a flare, no NSAIDs, no history of ulcers. My GI doc said, ‘You’re fine.’ And I felt better without it - no weird stomach stuff, no bloating. Just… normal. Why do we still do this? 🤷♂️
Allison Reed
November 30, 2025 AT 13:10
Thank you for sharing this. So many patients are scared to question their prescriptions - but you’ve laid it out clearly, calmly, and with evidence. That’s rare. If you’re on steroids and wondering if you need a PPI, you’re not alone. And you’re right to ask. Your body deserves better than blanket protocols.
Jacob Keil
December 1, 2025 AT 11:10
PPIs are just corporate magic pills sold to scared people who think their stomach is a warzone. Reality is your gut is way tougher than Big Pharma wants you to believe. Doctors prescribe them because they’re paid to push pills not think. H pylori is the real villain. But nobody wants to test for it. Too much work. Too little profit.
Rosy Wilkens
December 3, 2025 AT 09:55
Have you considered that this is all a ploy by the pharmaceutical industry to create dependency? PPIs are a gateway drug to lifelong medication. The FDA is complicit. The CDC ignores long-term risks. And now they’re pushing this narrative to make you believe you don’t need protection - but what if it’s a trap? What if the next study says PPIs prevent cancer? You’ll be sorry you stopped.
Andrea Jones
December 3, 2025 AT 21:02
Okay but like… I get why doctors do it. It’s easier to write a script than to have a 20-minute conversation about risk factors. But you’re right - it’s lazy medicine. I told my rheumatologist I didn’t want a PPI unless I was on ibuprofen. She actually paused. Then said, ‘You’re the first patient who’s ever asked for evidence.’ 👏
Justina Maynard
December 4, 2025 AT 11:05
My mom’s on prednisone for lupus, no NSAIDs, no ulcers, but she’s been on omeprazole for five years. She’s got osteoporosis now. And she’s 62. I showed her your post. She cried. Not because she’s scared - but because she realized she was told to take it ‘just in case’ and nobody ever told her the ‘in case’ was a myth. Thank you for giving her back her agency.
Evelyn Salazar Garcia
December 5, 2025 AT 15:44
PPIs are useless for steroids. Stop it.
Clay Johnson
December 6, 2025 AT 23:41
The system rewards volume not vigilance. Doctors don’t have time to audit each prescription. So they default. But default isn’t evidence. Evidence is what matters. And evidence says no.
Jermaine Jordan
December 8, 2025 AT 17:09
This isn’t just a medical update - it’s a revolution in patient empowerment. For decades, we’ve been told to swallow pills without question. But now? We’re waking up. We’re asking: ‘Why?’ We’re demanding proof. And for the first time, the science is on our side. This is how change happens - one patient, one question, one no at a time. Thank you for lighting the fire.