More than 10% of people in the U.S. say they’re allergic to penicillin. But here’s the twist: up to 90% of them aren’t. That’s not a typo. Most people who think they’re allergic to penicillin can safely take it again-after proper testing. The same goes for NSAIDs like ibuprofen or aspirin. The problem isn’t always an allergy. It’s often a side effect, a rash from a virus, or a misdiagnosis from years ago. And because of that, many people end up on stronger, more expensive, and riskier antibiotics. That’s not just inconvenient-it’s dangerous.
What Really Counts as a Drug Allergy?
A true drug allergy is an immune system reaction. It’s not just nausea, dizziness, or a mild rash. It’s your body treating a medicine like a threat. Symptoms show up fast-within minutes to an hour after taking the drug. Think hives, swelling of the lips or tongue, trouble breathing, dropping blood pressure, or anaphylaxis. These are real, life-threatening events. But here’s what most people don’t know: a stomachache after taking ibuprofen? That’s not an allergy. A headache after amoxicillin? Probably not either. Many so-called "allergies" are just side effects. The immune system isn’t involved. That’s why so many people get mislabeled. And once you’re labeled allergic, it sticks. Doctors avoid the drug. You get alternatives. Costs go up. Risks go up.Penicillin Allergy: The Most Common Misdiagnosis
Penicillin is the most reported drug allergy in history. But it’s also the most overdiagnosed. Skin testing is the gold standard for checking if you’re truly allergic. It’s simple: a tiny drop of penicillin is placed on your skin, then lightly pricked. If you react-redness, swelling-you might be allergic. But here’s the catch: up to 70% of positive skin tests are only to a component called PPL (Prepared Penicillin Polylysine). And those people? They can often still take penicillin without issue. If the skin test is negative, doctors often give a full dose of amoxicillin under supervision. If there’s no reaction? You’re cleared. No more "penicillin allergy" on your chart. That’s not just a relief-it’s a game-changer. Patients who get retested and cleared are far less likely to get broad-spectrum antibiotics like vancomycin or clindamycin. Those drugs cost more, cause more diarrhea, and raise the risk of C. diff infections.NSAID Allergies: Different Mechanism, Same Problem
NSAID allergies work differently. Penicillin allergies are usually IgE-mediated-your body makes antibodies. NSAID reactions? Often not. They’re more like pharmacological intolerance. Your body can’t handle the drug’s effect on prostaglandins. That’s why people with asthma or nasal polyps often react to aspirin or ibuprofen. Symptoms can include wheezing, nasal congestion, or hives. It’s not always an allergy in the classic sense, but it still needs to be taken seriously. Desensitization for NSAIDs is different too. Instead of a one-time IV protocol, it’s often daily dosing. Start with 30 mg of aspirin. Wait. Increase to 60 mg. Then 100 mg. Then 150 mg. Eventually, you reach 325 mg. Do this every day, and your body learns to tolerate it. This isn’t just for pain relief. It’s critical for people with heart disease who need daily aspirin to prevent clots. If you think you’re allergic, you might be denying yourself lifesaving care.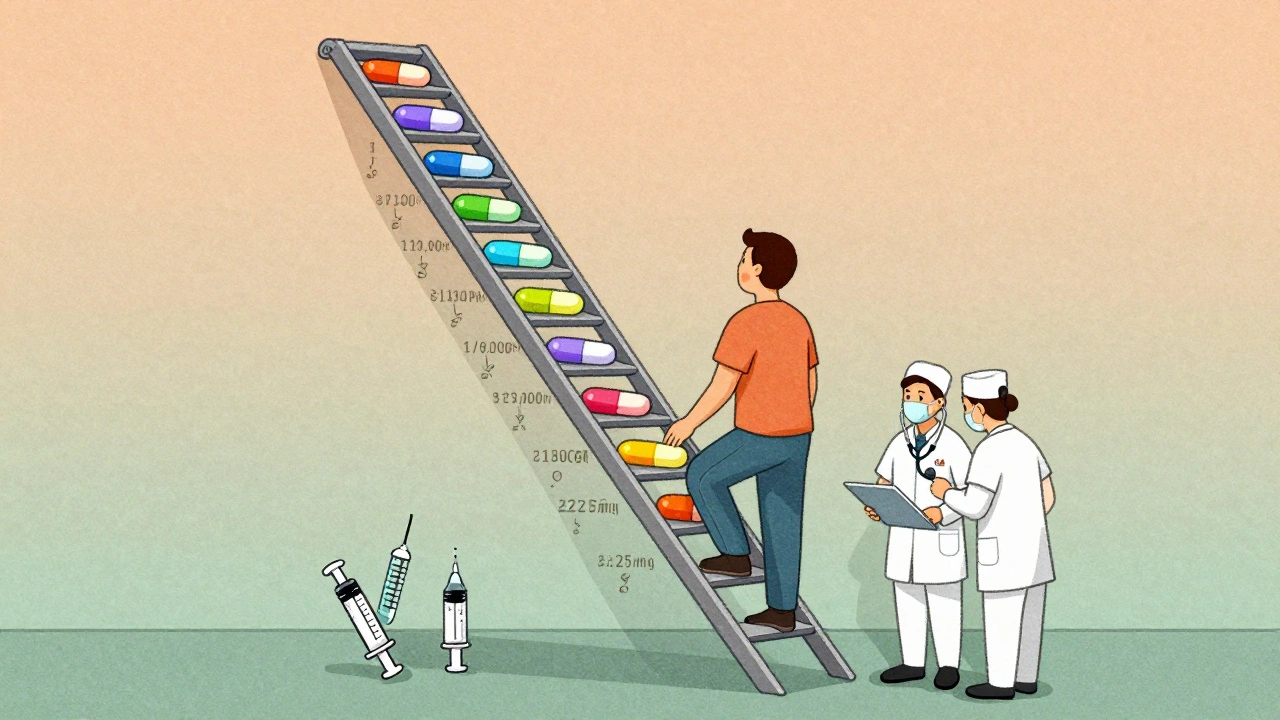
Desensitization: How It Works
Desensitization isn’t a cure. It’s a temporary reset. You’re not becoming immune. You’re just training your body to tolerate the drug-for one course of treatment. After that, you’re back to square one. If you need the drug again next year? You go through it all over again. The most common method is the 12-step protocol. It starts with a dose so tiny-1/10,000th of the full amount-it’s unlikely to trigger a reaction. Every 15 to 20 minutes, the dose doubles. It’s slow. It’s controlled. It’s done in a hospital, with emergency equipment ready. Epinephrine on standby. Nurses trained. The whole thing can take 4 to 8 hours. But for some drugs, like certain cephalosporins, it can be done in under 2.5 hours. It’s not just for penicillin. It’s used for chemotherapy drugs like paclitaxel, antifungals like fluconazole, and even monoclonal antibodies. The key? No good alternatives. If you have a life-threatening infection and every other antibiotic fails? Desensitization is your only shot.Who Gets Desensitized? And Who Doesn’t?
Not everyone qualifies. You need two things: a confirmed immediate reaction (within an hour) and no safe alternatives. If you had anaphylaxis after penicillin, you’re a candidate. If you just got a rash and took a different antibiotic that worked? You’re not. Children are a big gap here. Most protocols were designed for adults. Kids get the same doses, the same steps-but we don’t know if they’re optimal. Pediatric allergists, oncologists, and infectious disease specialists need to work together. Right now, too many kids are denied effective treatments because there’s no clear pediatric protocol. And here’s the hard truth: desensitization isn’t available everywhere. You need an allergy department with experience. Not every hospital has it. Not every doctor knows how to do it. That’s why so many people stay labeled allergic-even when they’re not.
Risks and Limits
Desensitization is safe when done right. But it’s not risk-free. About 1 in 10 people will have a mild reaction during the process-itching, flushing, a little wheezing. That’s usually manageable. But if your blood pressure drops hard or your throat swells shut? The procedure stops. Epinephrine is given. You’re treated. And you don’t try again that day. There’s also a small chance-about 2%-that you’ll become allergic again after re-exposure, especially if you got the drug through an IV. That’s why some experts recommend repeat skin testing before re-desensitizing, especially after a severe reaction. And yes, it’s expensive. It takes hours of staff time. Equipment. Monitoring. But compare that to the cost of treating a C. diff infection, a prolonged hospital stay, or a resistant infection. The savings are real.What Comes Next?
The field is moving. More hospitals are setting up desensitization programs. More guidelines are being written. But we still lack standardization. What works in Boston might not be used in Sydney. Pediatric protocols? Still mostly adapted from adult ones. That’s not good enough. The future? Better testing. Faster protocols. More collaboration between allergists, infectious disease doctors, and oncologists. And most importantly-better education. Patients need to know: "I think I’m allergic" doesn’t mean you are. And if you are, there’s a way forward. If you’ve been told you’re allergic to penicillin or an NSAID-especially if it was years ago-ask for a referral to an allergist. Get tested. Don’t assume the label is correct. You might be avoiding a safe, effective, cheaper drug for no reason.Frequently Asked Questions
Can I outgrow a penicillin allergy?
Yes. Many people lose their penicillin allergy over time-even if they had a serious reaction as a child. Studies show that 80% of people who were allergic 10 years ago can tolerate penicillin now. The best way to find out? Skin testing followed by a supervised drug challenge. Don’t assume it’s permanent.
Is NSAID desensitization safe for people with asthma?
Yes, but it must be done carefully. People with asthma and nasal polyps are more likely to have severe reactions to NSAIDs. Desensitization is one of the few ways they can safely take aspirin for heart protection. Protocols start with very low doses and are done under close monitoring. It’s not risk-free, but for many, it’s life-changing.
Can I do desensitization at home?
No. Desensitization must be done in a hospital or specialized clinic with immediate access to emergency care. Even mild reactions can turn serious fast. Epinephrine, oxygen, and trained staff must be available. Never attempt this on your own.
What if I had a reaction to one penicillin-does that mean I’m allergic to all antibiotics?
Not necessarily. Penicillin and related drugs like amoxicillin are in the same family, but other antibiotics like cefazolin or ceftriaxone are different. Cross-reactivity is low-around 1-3% for newer cephalosporins. Skin testing and careful challenges can tell you which ones are safe. Don’t avoid all antibiotics because of one reaction.
How long does the effect of desensitization last?
Only as long as you keep taking the drug daily. If you stop for more than 48 hours, your tolerance fades. If you need the drug again later-for another infection or surgery-you’ll need to go through desensitization again. It’s temporary, but it works when you need it most.

Annie Gardiner
December 6, 2025 AT 22:01
I used to think I was allergic to penicillin because I got a rash when I was six. Turns out it was chickenpox. Now I take amoxicillin like it’s candy. Why do we still treat medical labels like religious dogma? We don’t keep ‘gluten allergy’ on our records after 30 years of eating bread just fine. Time to stop letting old charts dictate our health.
Also, why is it that the moment someone says ‘allergy,’ everyone panics? It’s not a death sentence. It’s a misdiagnosis waiting to be corrected.
Rashmi Gupta
December 7, 2025 AT 15:54
My cousin in Delhi was told she’s allergic to ibuprofen after a headache. She’s been taking paracetamol for 12 years. Last month, she tried aspirin under supervision-nothing happened. Turns out her asthma was the trigger, not the drug. India’s hospitals don’t even test for this. We just avoid and suffer. Why is this not common knowledge?
Kumar Shubhranshu
December 9, 2025 AT 13:00
Most penicillin allergies are fake. Testing is free in some places. Stop being lazy. Get checked.
Mayur Panchamia
December 10, 2025 AT 22:04
Americans think they’re allergic to everything because they eat too much sugar and don’t walk anymore. In India, we don’t have time for fake allergies-we have real problems. If you can’t take penicillin, take the alternative. Stop making everything a medical drama. Your body is not a drama queen.
Kenny Pakade
December 11, 2025 AT 18:03
This is why America is broken. You get a rash at 8 and now you’re labeled allergic for life? No one checks? No one questions? This is why our healthcare costs are insane. We treat symptoms like sins. Fix the system, not the labels.
Gwyneth Agnes
December 12, 2025 AT 16:21
If you're allergic, you're allergic. Don't risk your life because you're too lazy to get tested. People die from anaphylaxis.
Ashish Vazirani
December 14, 2025 AT 03:37
My uncle in Mumbai was told he was allergic to penicillin after a fever in 1987. He was 19. Last year, at 62, he had sepsis. Vancomycin gave him kidney failure. They finally tested him-negative. He got amoxicillin. He’s home now. This isn’t just about money. It’s about dignity. We don’t let people die because of a 40-year-old chart error.
And yes, I cried. Not because I’m emotional. Because this system is broken.
Kay Jolie
December 15, 2025 AT 23:15
It’s fascinating how the biomedical paradigm has pathologized pharmacological tolerance as immunological hypersensitivity. The IgE-mediated paradigm is so reductive-it fails to account for non-IgE-mediated pharmacodynamic intolerance, particularly in NSAID-induced bronchospasm, which is a prostaglandin dysregulation phenomenon, not an allergy per se.
And yet, the clinical inertia persists. We’re still operating on binary labels in a multivariate world. Desensitization protocols? They’re not just therapeutic-they’re epistemological interventions. We’re literally rewriting biological narratives through controlled exposure.
But let’s be honest: the infrastructure for this is laughably uneven. In rural America? Forget it. In tertiary centers? Maybe. This isn’t medicine. It’s privilege.
Max Manoles
December 16, 2025 AT 21:01
Just got my penicillin skin test results back-negative. Did the amoxicillin challenge today. No reaction. My chart now says ‘penicillin allergy: ruled out.’ It feels weird to type that. I’ve avoided it since I was 7.
Also, my insurance saved $2,100 on this one infection because I didn’t need vancomycin. The hospital didn’t charge me for the test. That’s the kind of thing that should be standard. Not a luxury.
Arjun Deva
December 17, 2025 AT 07:06
They’re lying. All of it. Penicillin allergies are a Big Pharma trick to sell you expensive antibiotics. The ‘desensitization’? That’s just a way to get you hooked on hospital visits. They want you to keep coming back. Why else would they push this so hard?
And why do you think they don’t test kids? Because they’re easier to label. Once you’re labeled, you’re a customer for life. The CDC? The WHO? All in on the scam. I’ve seen the documents. They know.
Don’t trust the system. Don’t trust the ‘experts.’ You think your rash was an allergy? It was a warning. Listen to your body. Not your doctor.