Patient Hesitation: Why People Delay Medication and How to Fix It
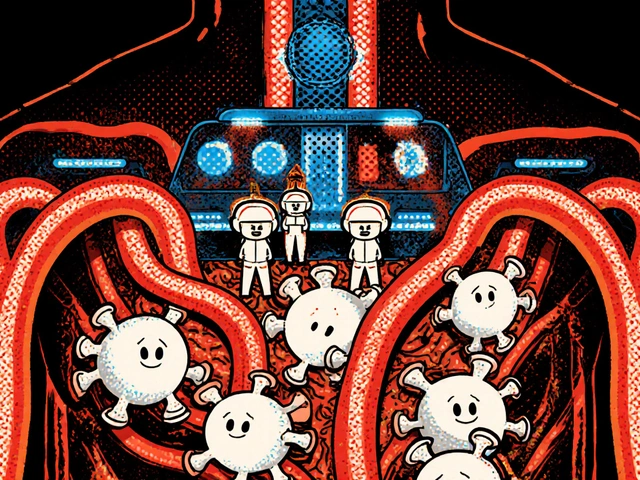
When someone avoids taking a prescribed drug—even when it could help—they’re not being stubborn. They’re responding to real fears, misinformation, or past experiences. This is patient hesitation, the delay or refusal to start, continue, or take medication as directed due to fear, misunderstanding, or negative expectations. Also known as medication non-adherence, it’s not just about forgetting pills—it’s about distrust in the system, confusion over side effects, or believing the drug won’t work. Studies show up to half of patients don’t take their meds correctly, and in many cases, it’s not because they’re careless. It’s because they’ve heard horror stories, seen misleading ads, or had a bad reaction they didn’t understand.
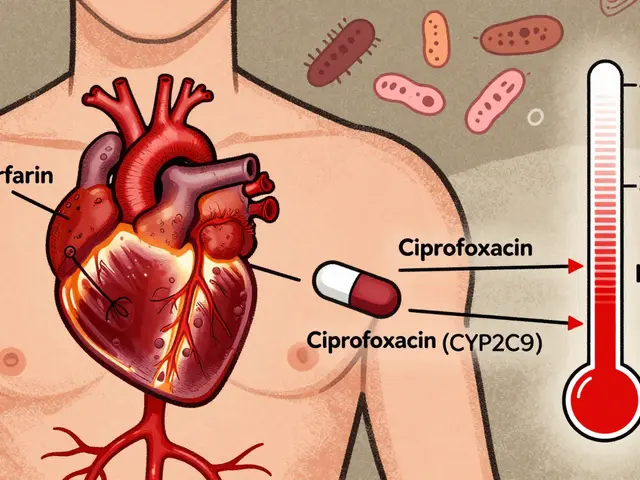
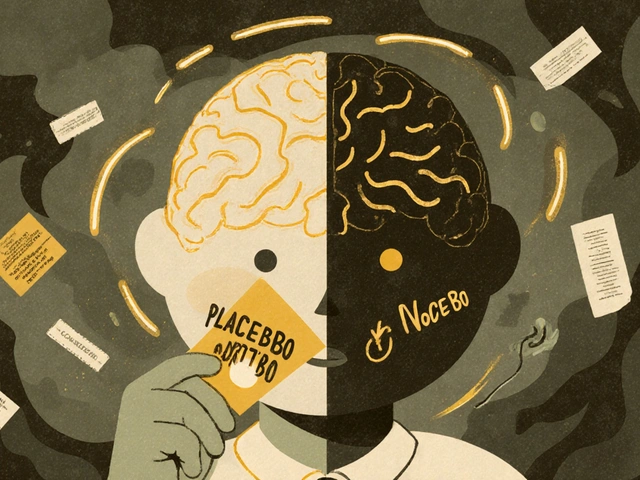
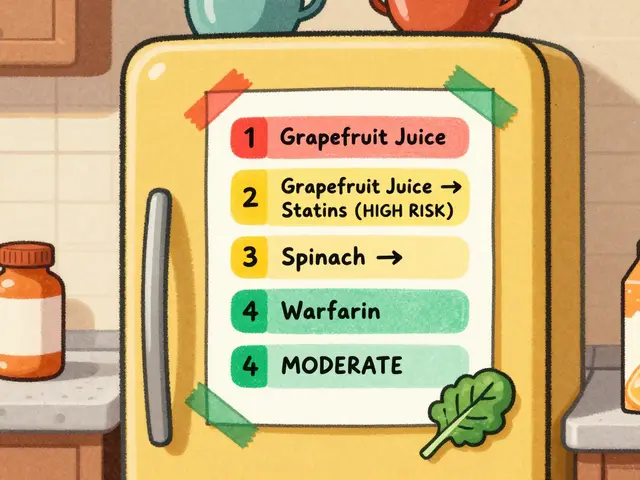
drug side effects, unwanted physical or mental responses to medication often fuel this hesitation. A person might stop taking a statin because they heard it causes muscle pain, not realizing that most reported pain isn’t actually from the drug. Or they skip antibiotics after hearing about yeast infections, not knowing that the risk is low and manageable. Meanwhile, treatment expectations, what a patient believes will happen when they take a drug can be just as powerful as the drug itself. The placebo effect, when a person feels better because they expect to is well-known—but the nocebo effect, when a person feels worse because they expect to is rarely discussed. If you tell someone their pill might cause dizziness, they’re far more likely to feel dizzy—even if it’s a sugar pill.
Real cases show this isn’t theoretical. Someone on warfarin avoids alcohol not because it’s dangerous, but because their pharmacist said "never drink"—even though moderate amounts are fine. A person with Graves’ disease refuses selenium because they think it’s "just a supplement," not knowing it reduces thyroid antibodies. Others avoid generics because they believe brand names are stronger, even when providers confirm they’re identical. These aren’t irrational choices—they’re logical responses to unclear information.
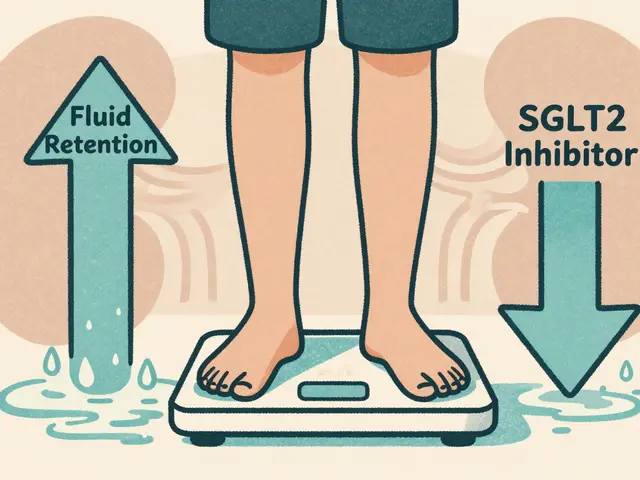
The fix isn’t more warnings or louder prescriptions. It’s clearer communication, honest conversations about risk, and helping patients understand what’s real and what’s rumor. When people know why a drug is prescribed, what side effects actually mean, and how to spot real danger versus normal adjustment, hesitation drops. The posts below show how these issues play out in real life—from corticosteroids and alcohol interactions to how smoking changes clozapine levels and why splitting pills can backfire if done wrong. You’ll see what patients get wrong, what providers see daily, and how simple changes in how we talk about meds can make a huge difference.