Hypersensitivity Protocols: What They Are and How They Keep You Safe
When your body overreacts to something harmless—like a penicillin shot or a bee sting—it’s not being dramatic. It’s triggering a hypersensitivity protocol, a structured system designed to identify, manage, and prevent dangerous immune overreactions to drugs, foods, or environmental triggers. Also known as allergy management plans, these protocols are the difference between a mild rash and a life-threatening anaphylaxis, a sudden, severe allergic reaction that can shut down breathing and circulation. They’re not optional in hospitals, clinics, or even pharmacies—they’re built into daily practice because the stakes are too high to guess.
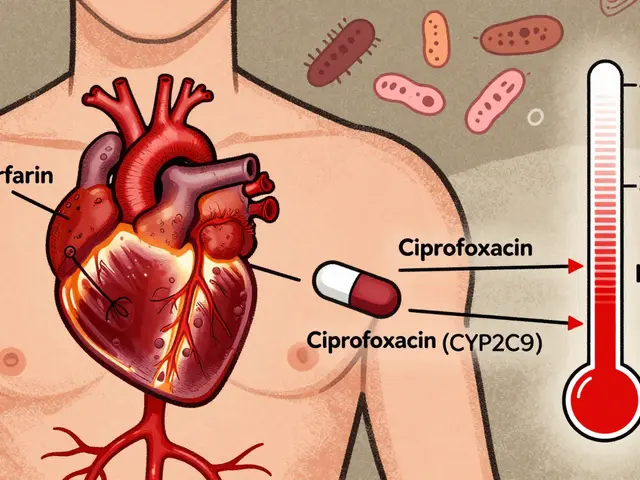
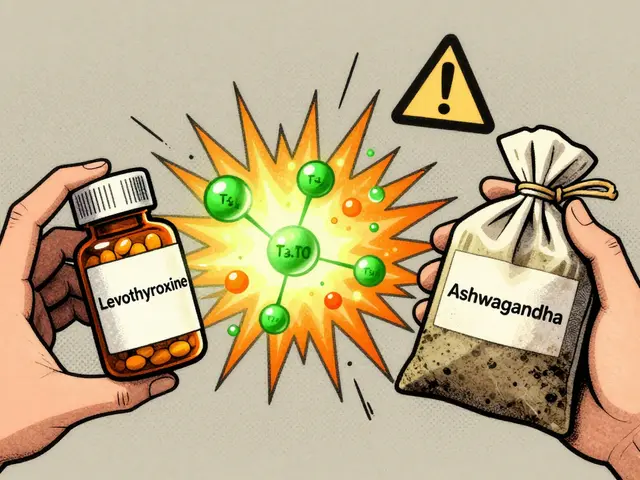
Hypersensitivity protocols aren’t just about avoiding the obvious triggers. They’re about understanding patterns. For example, if someone had a reaction to one drug hypersensitivity, an immune-mediated adverse reaction to a medication that isn’t dose-dependent and often mimics an allergy to amoxicillin, they might also react to other beta-lactam antibiotics. Protocols help clinicians map these connections using skin tests, challenge doses, and detailed patient histories. They also account for cross-reactivity—like how sulfa drugs can trigger reactions in people who think they’re only allergic to penicillin. And it’s not just about drugs. These same principles apply to contrast dyes used in CT scans, latex gloves, and even some food additives in medications. The goal isn’t to scare you, but to give you a clear path forward when your body says "no."
What makes a good protocol? It’s not just a checklist. It’s a conversation. It’s asking: "Have you ever had trouble breathing after taking a pill?" It’s knowing that a rash that showed up two weeks after starting a new medicine might be more serious than a simple irritation. It’s having naloxone or epinephrine ready—not because you expect it to be used, but because you’re prepared if it is. These protocols are shaped by real cases: the patient who got anaphylaxis from a generic version of a drug they’d taken safely before, the nurse who caught a delayed reaction because they knew to watch for fever and joint pain, the pharmacist who flagged a drug interaction because the patient mentioned a past reaction to a similar compound.
You’ll find posts here that dig into how these systems work in practice—how hospitals track reactions, how pharmacists adjust prescriptions, and how patients can speak up before it’s too late. Some cover the science behind why your immune system turns on a drug. Others show how to recognize early signs you might miss. There’s no magic bullet, but there are clear steps. And if you’ve ever been told "you’re allergic to something" without knowing what that really means, this collection is for you.