The U.S. pharmaceutical supply chain handles over 5 billion prescription drug transactions every year. That’s a lot of pills, injections, and vials moving from manufacturers to pharmacies. And for decades, there was no reliable way to know if any of those drugs were fake, stolen, or tampered with. Counterfeit drugs don’t just waste money-they can kill. A fake version of a blood thinner, insulin, or cancer drug could contain the wrong dose, toxic chemicals, or nothing at all. In 2013, Congress passed the Drug Supply Chain Security Act (DSCSA) a federal law requiring electronic, interoperable tracking of prescription drugs from manufacturer to pharmacy to fix that. By November 27, 2024, every single package of prescription medicine in the U.S. must have a unique digital fingerprint. This isn’t just paperwork. It’s a full-system overhaul designed to stop counterfeit drugs before they reach your medicine cabinet.
What Exactly Is the DSCSA?
The DSCSA didn’t come out of nowhere. It was a direct response to real-world dangers. In the early 2010s, investigators found counterfeit versions of popular drugs like Avastin and Lovenox being sold through shady online pharmacies and unlicensed distributors. Some had no active ingredient. Others had dangerous fillers. The problem wasn’t just illegal websites-it was that legitimate-looking wholesalers and pharmacies were unknowingly handling fake drugs because there was no way to verify them. Before DSCSA, each state had its own rules. Some required paper records. Others didn’t require anything at all. That patchwork made it easy for bad actors to slip through the cracks. The DSCSA created one national standard. It says every prescription drug package must have a unique serial number, a barcode, and a clear label with the National Drug Code (NDC), lot number, and expiration date. That’s the product identifier. It’s not just a barcode-it’s a digital ID that can be scanned and verified at every step. The law also requires every company in the supply chain-manufacturers, repackagers, wholesalers, and pharmacies-to share electronic data about each package as it changes hands. This includes three key pieces of information: Transaction Information (what the product is), Transaction History (where it’s been), and Transaction Statement (proof it’s legitimate). Together, they form an electronic pedigree that can’t be forged.How the System Works: From Factory to Pharmacy
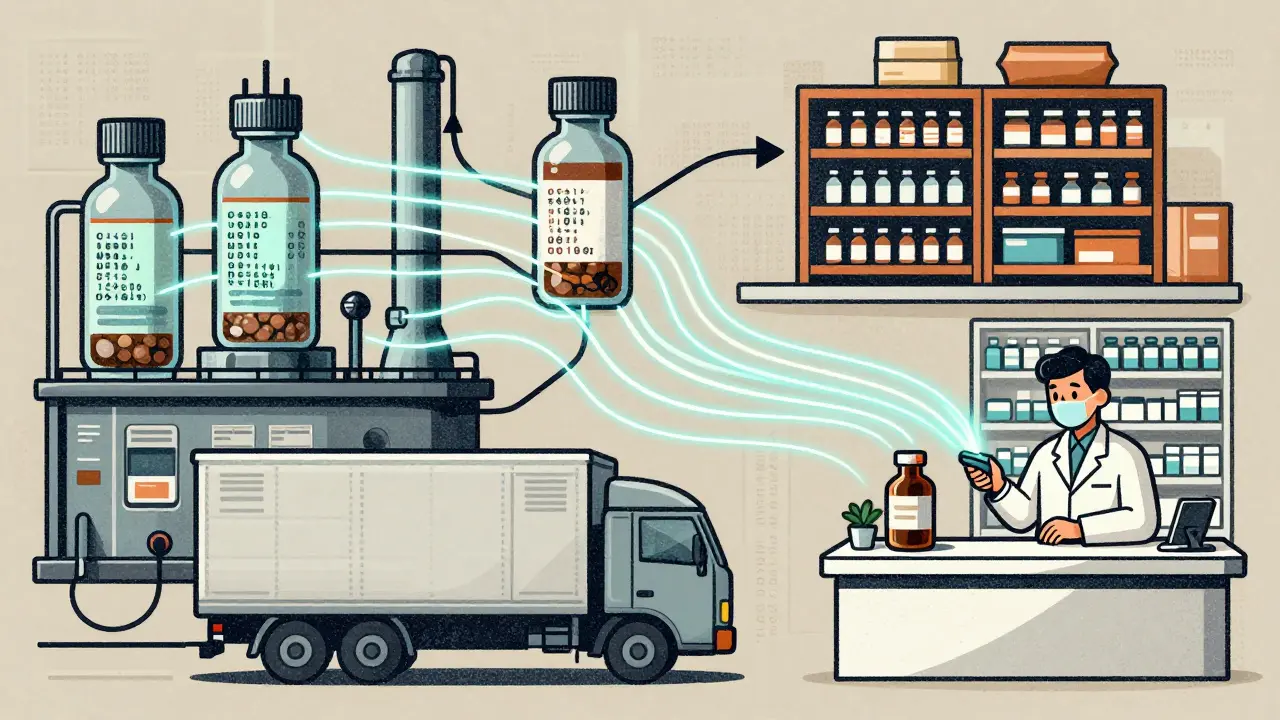
Here’s how it actually works on the ground. A manufacturer like Pfizer or Merck prints a unique 20-character serial number on each pill bottle or vial using GS1 standards. That number is linked in their system to the product’s NDC, lot, and expiration date. When the drug leaves the factory, the manufacturer sends an electronic record to the next partner-usually a wholesaler like McKesson or Cardinal Health. That record includes the serial number, the date of sale, and the destination. When the wholesaler ships it to a pharmacy, they send another record. And when the pharmacy receives it, they scan the barcode and check the serial number against the manufacturer’s database in real time. If the serial number doesn’t match, or if it’s been used before, the system flags it as a suspect product. That triggers an investigation. The pharmacy can’t dispense it. They must quarantine it and report it to the FDA. This isn’t hypothetical. In 2022, a regional distributor got a warning letter from the FDA for failing to do exactly that. They had received a package with a duplicated serial number but didn’t investigate. That’s exactly the kind of failure DSCSA was built to prevent. The system also allows for pinpoint recalls. Before DSCSA, if one bad lot of a drug was found, companies had to recall entire product lines-sometimes millions of units. Now, they can target just the affected serial numbers. CVS Health reported a 75% drop in suspect product investigations after implementing automated verification systems. That’s faster, cheaper, and safer for patients.Why This Matters for Patients
You might think, “I don’t buy drugs online. I’m safe.” But counterfeit drugs don’t always come from shady websites. They can enter the legitimate supply chain through stolen shipments, diverted inventory, or fake paperwork. A 2021 FDA study estimated that counterfeit drugs accounted for up to 1% of the U.S. market-about $10 billion worth. That’s not just a financial loss. It’s a public health risk. DSCSA’s track-and-trace system cuts that risk by up to 95%, according to FDA estimates. How? Because every package can be traced back to its source. If a drug is found to be fake, investigators can follow the digital trail to find where it entered the system. Was it stolen from a warehouse? Was it repackaged illegally? Was it shipped from a foreign supplier without authorization? The data gives them answers. For patients, that means fewer surprises. No more wondering if your blood pressure medication is real. No more risk of getting a counterfeit version of a life-saving drug. And if something does go wrong, the system makes it easier to act fast. The FDA can issue targeted alerts instead of blanket warnings. Pharmacies can verify drugs before they go on the shelf. And if a drug is pulled, it’s not because of a broad recall-it’s because a specific serial number was flagged. That’s precision, not panic.
Who’s Complying-and Who’s Struggling
The DSCSA deadline is November 27, 2024. And the industry is racing to get ready. Manufacturers are ahead of the curve. Nearly 98% have implemented serialization. Wholesalers are close behind at 95%. But pharmacies? Only 72% of all pharmacies are fully compliant. And here’s the catch: chain pharmacies like Walgreens and CVS have it mostly figured out. They spent over $120 million each on technology upgrades. But independent pharmacies? They’re struggling. A 2023 survey by the National Community Pharmacists Association found that 68% of independent pharmacies say DSCSA compliance is their biggest tech challenge. Why? Cost. Upgrading systems can run $100,000 to $185,000 per pharmacy. That’s a huge investment for a small business. Many still rely on old software that can’t talk to new DSCSA platforms. Data mismatches are common-serial numbers don’t match between systems, lot numbers are entered wrong, or transaction histories are incomplete. That causes delays. Some pharmacies report waiting 2-3 days just to verify a shipment. That’s not just frustrating-it’s dangerous if a patient needs medication right away. The biggest technical hurdle? Interoperability. There are over 40 software vendors offering DSCSA solutions-TraceLink, SAP, Oracle, and others. But not all of them speak the same language. Even if two companies use EPCIS standards (the data format required for interoperability), their systems might still have trouble exchanging information. The FDA has given the industry a one-year stabilization period after the deadline to fix these glitches without penalties. But they’re clear: full compliance is non-negotiable by November 2024.What Happens After November 2024?
The DSCSA isn’t the end-it’s the beginning. The FDA is already looking ahead. In March 2023, Commissioner Dr. Robert Califf told Congress the agency is evaluating whether to extend track-and-trace requirements to certain over-the-counter (OTC) drugs. Think pain relievers, allergy meds, or sleep aids-products that are often targeted by counterfeiters because they’re sold without a prescription. Long-term, the system is expected to save the industry $2.3 billion a year. How? Fewer recalls, less drug diversion, and lower fraud. PwC projects counterfeit drug incidents will drop by 90% by 2027. That’s not just a win for companies-it’s a win for patients. And as the technology matures, it’s becoming more automated. AI tools now help flag suspicious patterns in transaction data. Blockchain pilots are being tested to make records even more tamper-proof. But the real success of DSCSA won’t be measured in software sales or compliance reports. It’ll be measured in lives saved. When a pharmacist scans a bottle and knows, with absolute certainty, that the medicine inside is real-that’s the power of this system. It turns a fragmented, vulnerable supply chain into a secure, transparent network. And for the first time in U.S. history, every prescription drug has a digital paper trail. No more guessing. No more hidden risks. Just clear, verifiable safety.
Common Misconceptions
Some people think DSCSA is just about barcodes. It’s not. Barcodes are just the visible part. The real work is in the electronic data exchange-what’s sent between companies, how it’s verified, and how it’s stored. Others believe the system is already fully operational. It’s not. While most manufacturers are compliant, the final step-full interoperability between all trading partners-is still being ironed out. Another myth: DSCSA is the same as the EU’s Falsified Medicines Directive. It’s not. The EU requires anti-tamper seals and a central database. The U.S. system is decentralized-it relies on direct communication between companies, not a single government database. That makes it more flexible but also more complex to coordinate. And no, this isn’t just a U.S. problem. Counterfeit drugs are a global issue. But DSCSA is one of the most advanced systems in the world. It’s setting a new standard.What happens if a pharmacy can’t verify a drug’s serial number?
If a pharmacy scans a drug and the serial number doesn’t match the manufacturer’s database, or if it’s been used before, the system flags it as a suspect product. The pharmacy must immediately stop dispensing it, quarantine it securely, and report it to the FDA. They’re also required to investigate the source-was it stolen? Was it repackaged illegally? The FDA expects a full report within 24 hours. Failure to do so can result in fines or enforcement action.
Is DSCSA only for prescription drugs?
Yes, for now. The DSCSA applies only to prescription drugs distributed in the U.S. But the FDA has publicly stated it’s evaluating whether to extend the requirements to certain high-risk over-the-counter medications, like insulin pens, epinephrine auto-injectors, or sleep aids that are frequently counterfeited. No official decision has been made yet, but expansion is likely in the next few years.
How much does DSCSA compliance cost a small pharmacy?
For independent pharmacies, the average cost to become DSCSA-compliant ranges from $150,000 to $185,000. This includes new software, barcode scanners, staff training, and integration with wholesalers’ systems. Many small pharmacies struggle with this expense, and some have delayed compliance due to budget constraints. Grants and vendor payment plans are available, but they don’t cover everything.
Do I need to do anything as a patient?
No. You don’t need to scan barcodes or check serial numbers. The system works behind the scenes. Your pharmacist and the supply chain partners handle verification. Your only job is to get your medication from a licensed pharmacy. If you ever receive a drug that looks odd-different color, smell, or packaging-report it to your pharmacist. They’re trained to spot and report suspect products.
Why are some companies still having trouble with DSCSA?
The biggest issues are outdated legacy systems that can’t communicate with newer platforms, inconsistent data entry (like typos in lot numbers), and differences in how vendors implement EPCIS standards. Even if two companies use the same software, their data formats might not align perfectly. These mismatches cause delays in verification, sometimes holding up shipments for days. The FDA’s stabilization period is meant to give companies time to fix these problems without penalties.
What happens after the November 2024 deadline?
After November 27, 2024, full electronic traceability becomes mandatory. The FDA will no longer exercise enforcement discretion. Companies that haven’t met the requirements will face penalties, including fines, product seizures, or loss of licensing. The focus will shift from implementation to ongoing compliance-ensuring systems stay accurate, secure, and interoperable. The FDA will also begin monitoring for new threats, like digital counterfeiting or data spoofing.
Mindee Coulter
January 27, 2026 AT 22:07
Finally something that actually works. I work in a hospital pharmacy and we’ve been scanning everything since 2022. No more guessing if a bottle came from a shady distributor. The system catches duplicates in seconds. Game changer.
Rhiannon Bosse
January 28, 2026 AT 17:37
Oh wow so now the government is tracking every pill I take? 😏 Next they’ll put a chip in my insulin pen. Who’s really behind this? Big Pharma + FDA + Silicon Valley. This isn’t safety-it’s control. And don’t even get me started on how they’re forcing small pharmacies out with $185k tech bills. Capitalism with a side of tyranny.
Colin Pierce
January 30, 2026 AT 03:04
Actually, the cost breakdown for independent pharmacies is way worse than people realize. It’s not just software-it’s training, hardware, IT support, and the fact that half your staff quits because they can’t figure out the new scanners. I’ve seen clinics shut down over this. The FDA’s ‘stabilization period’ is a band-aid on a hemorrhage.
Lexi Karuzis
January 30, 2026 AT 13:54
And yet… you still can’t trust the data. I work in compliance. I’ve seen serial numbers match… but the lot number is wrong. Or the expiration date is off by a year. The system assumes everyone inputs data correctly. But humans? We’re messy. This is digital snake oil wrapped in a GS1 sticker.
Anna Lou Chen
January 31, 2026 AT 04:07
Let’s deconstruct the epistemological framework of DSCSA: it assumes that traceability equals safety, but safety is a phenomenological construct contingent upon institutional trust. The blockchain-adjacent architecture of EPCIS merely reifies the illusion of transparency-when in reality, it’s a performative act of regulatory theater designed to pacify public anxiety while enabling corporate consolidation. The real enemy isn’t counterfeit drugs-it’s the commodification of health itself.
Brittany Fiddes
February 1, 2026 AT 14:41
Of course the US is doing this right. The EU? They just slap on a tamper seal and call it a day. Pathetic. We’re building a digital fortress. The rest of the world is still using paper ledgers and prayers. We’re not just regulating drugs-we’re defining the future of global pharmaceutical integrity. Bow down to American innovation.
John Rose
February 1, 2026 AT 19:17
Interesting that the article mentions AI and blockchain pilots. Has anyone looked into whether those systems are vulnerable to adversarial attacks? What if someone generates a fake serial number that passes validation because the AI was trained on corrupted data? We’re building a very sophisticated trap for ourselves.
Mark Alan
February 2, 2026 AT 01:44
MY PHARMACY GOT A $200K BILL AND NOW I CAN’T GET MY ANTIBIOTICS IN 2 HOURS 😭😭😭
Ambrose Curtis
February 2, 2026 AT 05:01
Yeah but honestly? I’ve seen way more errors from big chain systems than small ones. CVS’s software glitches so bad they sometimes flag real bottles as fake. Meanwhile, my buddy’s mom’s independent pharmacy? They manually cross-check every lot number with a printed sheet. It’s slower but way less buggy. Tech ain’t always better.
Robert Cardoso
February 3, 2026 AT 05:34
95% reduction in counterfeit drugs? Where’s the peer-reviewed study? FDA estimates aren’t data-they’re PR. The 1% figure cited earlier is based on a 2021 survey of 120 samples. That’s not a statistically valid population. You can’t extrapolate national trends from a handful of bottles. This is fearmongering dressed as policy.
Linda O'neil
February 4, 2026 AT 23:13
Don’t give up on the small pharmacies! They’re the backbone of rural America. I know a guy in Nebraska who’s using a $500 tablet and an open-source scanner. It’s not perfect-but it’s working. We need grants, not blame. Let’s rally behind them.
Katie Mccreary
February 5, 2026 AT 03:37
So you’re telling me I can’t even trust my own meds? 😂
Amber Daugs
February 5, 2026 AT 10:46
And yet, the same people who scream about DSCSA costs are the ones who buy their insulin from Mexico. You want safety? Then stop being a hypocrite. If you’re not willing to pay for it, don’t complain when the system works. Your life isn’t a protest.