Kidney Medication Safety Checker
Check Your Medication Safety
Enter your current eGFR value and select medications you're taking to identify potential risks based on kidney function.
When your kidneys aren’t working right, your body can’t flush out medicines like it used to. That doesn’t mean you stop taking them-it means you have to take them differently. For millions with chronic kidney disease (CKD), the same dose that’s safe for a healthy person can become dangerous, even deadly. Medications pile up in the bloodstream, leading to confusion, heart rhythm problems, internal bleeding, or sudden kidney failure. And most of the time, it’s preventable.
Why Your Kidneys Matter for Medicines
Your kidneys don’t just make urine. They filter about 30% of all prescription and over-the-counter drugs out of your blood. When kidney function drops, those drugs stick around longer. Some don’t get broken down at all. Others build up slowly, like water filling a clogged sink. By the time you feel sick, the damage may already be done. The problem starts early. Once your estimated glomerular filtration rate (eGFR) falls below 60 mL/min/1.73m²-Stage 3 CKD-40% of commonly used drugs need a dose change. Yet, studies show that 35% of primary care doctors never calculate eGFR. They see a creatinine number and assume everything’s fine. It’s not.Top 5 Dangerous Medications for Kidney Patients
- NSAIDs (ibuprofen, naproxen, diclofenac): These painkillers cut blood flow to the kidneys. In someone with eGFR under 60, they triple the risk of acute kidney injury. One patient in Perth saw their creatinine jump from 1.8 to 3.2 after just two days of ibuprofen for back pain. They ended up hospitalized for five days.
- Metformin: The go-to diabetes drug. But if eGFR drops below 30, it can cause lactic acidosis-a rare but fatal buildup of acid in the blood. The fix? Stop it. Don’t just lower the dose. Many doctors still prescribe it at full strength in late-stage CKD. Don’t let that happen to you.
- Sulfonylureas (chlorpropamide, glyburide): These diabetes pills can cause dangerously low blood sugar that lasts for days. Chlorpropamide’s half-life stretches from 34 hours to over 200 hours in Stage 5 CKD. One patient had a seizure after taking a normal dose because their body couldn’t clear it.
- Trimethoprim (in co-trimoxazole): Used for urinary infections. But when combined with ACE inhibitors or ARBs (common for high blood pressure and kidney protection), it can spike potassium levels by 1.5 mmol/L in 48 hours. That’s enough to trigger heart arrhythmias. Many patients don’t know this combo is a ticking time bomb.
- Aciclovir: For herpes or shingles. At normal doses, it forms crystals in the kidney tubules. In someone with eGFR under 50, up to 15% develop crystal nephropathy. Symptoms? Confusion, seizures, vomiting. It looks like a stroke-but it’s just a drug that wasn’t adjusted.
What About Blood Thinners and Antibiotics?
Direct oral anticoagulants (DOACs) like apixaban and rivaroxaban are popular because they don’t need regular blood tests like warfarin. But here’s the catch: apixaban is 50% cleared by the kidneys. In Stage 4 CKD (eGFR 15-29), bleeding risk jumps 40% compared to healthy patients. Many doctors still prescribe standard doses. The fix? Switch to warfarin-or lower the DOAC dose based on eGFR and weight. Vancomycin, a powerful antibiotic used in hospitals, is another silent killer. Standard dosing is 15 mg/kg every 12 hours. But if your eGFR is under 30, you need that same dose only every 48 to 72 hours. If you don’t monitor blood levels, you can get permanent hearing loss or kidney damage. Yet, many hospitals still don’t check trough levels in CKD patients.
How Doctors Miss the Signs
It’s not just about forgetting to adjust doses. It’s about not knowing what to look for.- Doctors rely on serum creatinine alone-ignoring age, sex, and muscle mass. A 75-year-old woman with normal creatinine might have an eGFR of 35.
- Pharmacists don’t always flag high-risk combinations. A patient on lisinopril (an ACE inhibitor) gets a script for trimethoprim. No one connects the dots.
- Patients don’t speak up. They think, “If my doctor prescribed it, it’s safe.” But many don’t know their own eGFR. One survey found 78% of CKD patients received at least one unadjusted medication.
What You Can Do Right Now
You don’t need to be a doctor to protect yourself.- Know your eGFR. Ask for it at every visit. Write it down. If it’s under 60, assume every new medication needs a review.
- Keep a full medication list. Include vitamins, supplements, and OTC drugs. Bring it to every appointment. Highlight NSAIDs, painkillers, and antibiotics.
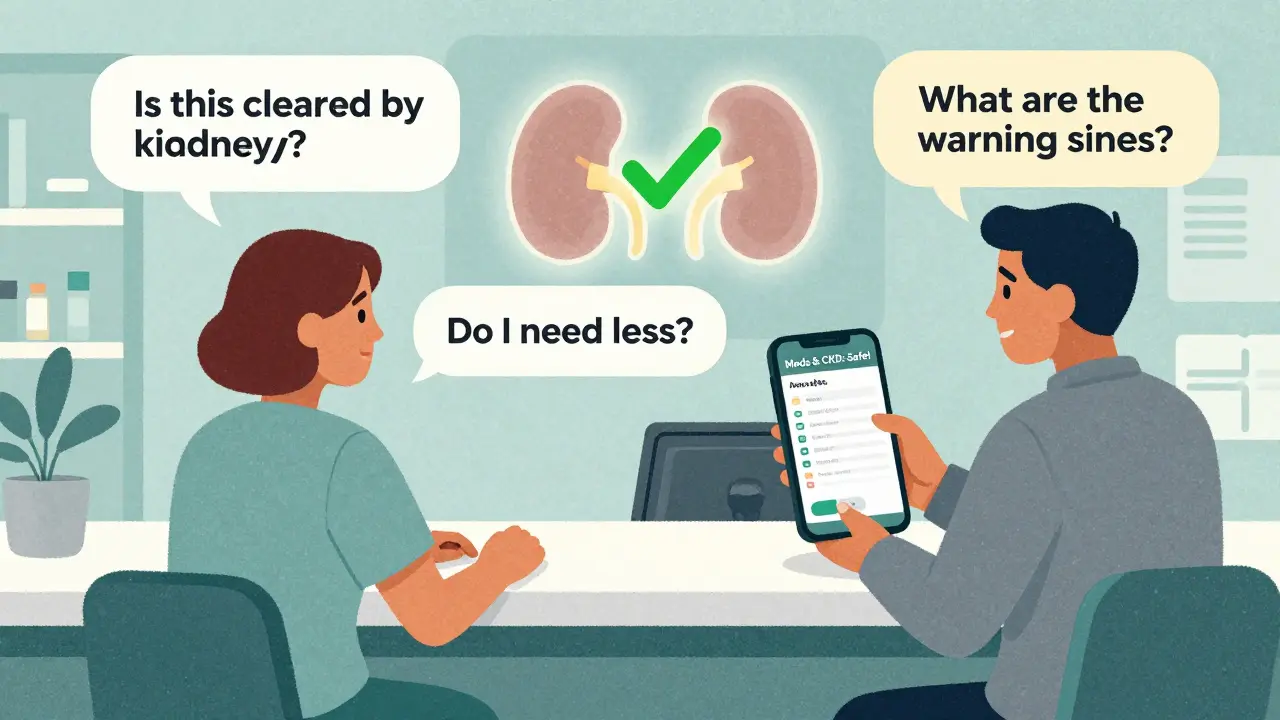
- Ask three questions: “Is this drug cleared by the kidneys?” “Do I need a lower dose?” “What are the warning signs if it’s too much?”
- Use a tool. Apps like Meds & CKD (from Healthmap Solutions) scan your meds and flag risks based on your eGFR. Users report 82% better communication with their doctors after using it.
- Never take NSAIDs without asking. Even a single dose of ibuprofen can trigger kidney injury in Stage 3 or worse. Use acetaminophen instead-unless you have liver disease.
New Tools Are Coming-But Don’t Wait
Technology is catching up. In 2023, the FDA approved KidneyIntelX, a machine learning tool that predicts your personal risk for drug toxicity with 89% accuracy. Electronic health records are starting to auto-flag unsafe prescriptions. Stanford researchers are testing gene-based dosing to personalize meds even further. But these tools aren’t everywhere. And even if they were, you’re still the best line of defense. The data is clear: 65% of medication-related kidney injuries are preventable. That means you have power.What Happens If You Ignore It?
Drug-induced acute kidney injury (AKI) happens in 14-26% of hospital cases involving kidney patients. Mortality? Up to 50% in severe cases. The average hospital bill? $12,000. And 38% of those cases could have been avoided with simple dose adjustments. One patient in Melbourne, 72, was on lisinopril, metformin, and a standard dose of naproxen for arthritis. She didn’t know her eGFR was 28. Within a week, she was in the ER with vomiting, confusion, and a potassium level of 6.8. She needed emergency dialysis. Her kidneys never fully recovered. It’s not a rare story. It’s routine.Final Thought: Your Kidneys Can’t Speak. You Can.
Kidney disease doesn’t always cause symptoms. That’s why it’s called the silent disease. But medication toxicity? That comes with warning signs-dizziness, nausea, irregular heartbeat, swelling, confusion. If you’re on multiple meds and have CKD, these aren’t just side effects. They’re red flags. Don’t wait for your doctor to catch it. Be the one who asks. Be the one who checks. Be the one who says, “I have kidney disease. Is this safe for me?”Because in this case, the most dangerous thing isn’t the disease. It’s the assumption that what’s safe for everyone is safe for you.
Alexandra Enns
January 24, 2026 AT 11:55
This is such a blatant case of medical negligence. My aunt in Toronto died because her doctor kept giving her ibuprofen even after her eGFR dropped to 22. They didn't even check her meds. It's not just ignorance-it's systemic. The system is designed to let people like her die so hospitals can keep billing for dialysis. Wake up, people.
Marie-Pier D.
January 24, 2026 AT 13:03
I'm so glad someone finally said this. 💔 My dad has CKD and I made him a printed meds list with red flags on NSAIDs and metformin. He showed it to his doctor and they actually changed his script. You don't need to be a doctor to save your own life. Just be loud. 🙏
Shanta Blank
January 25, 2026 AT 23:47
OMG I literally cried reading this. Like, full-on ugly sobbing. My sister got hospitalized last year after taking naproxen for her 'just a little back pain' and now she's on permanent dialysis. This isn't medical advice-it's a death sentence wrapped in a prescription bottle. #RIPToxicMedicine
Tiffany Wagner
January 27, 2026 AT 03:46
i had no idea trimethoprim and lisinopril could do that. i take both. im gonna call my pharmacist tomorrow. thanks for the heads up
Vatsal Patel
January 29, 2026 AT 02:27
Ah yes, the classic Western medical industrial complex. You think your kidneys are special? In India, we don't have eGFR machines. We have grandmas who know which herbs to avoid when the urine turns yellow. You don't need algorithms-you need humility. The West thinks it's advanced. It's just addicted to pills.
Sharon Biggins
January 31, 2026 AT 01:38
this really helped me feel less alone. i’ve been scared to ask my doctor about my meds because i dont want to seem like a pain. but now i know its my right to ask. thank you
John McGuirk
January 31, 2026 AT 19:44
You think this is bad? Wait till you find out the FDA approves these drugs because Big Pharma pays off the regulators. They don't care if you die. They just want your insurance number. Dialysis machines are a billion-dollar industry. Your kidney failure is their profit margin.
Michael Camilleri
February 2, 2026 AT 09:51
People like you think you can just 'ask questions' and fix this. Newsflash-your doctor doesn't have time. Your pharmacist doesn't care. Your insurance won't cover the tests. You're just a number in a system built to grind you down until you're too sick to fight. You think knowledge helps? It doesn't. It just makes you suffer longer.
lorraine england
February 3, 2026 AT 16:52
I'm a nurse and I see this every week. So many patients don't even know what eGFR means. I always write it on their discharge papers in big letters. You're not being paranoid-you're being smart. Keep asking. You're doing great.
Kat Peterson
February 4, 2026 AT 14:45
I literally just got prescribed co-trimoxazole yesterday 😭😭😭 and I have eGFR 31. I’m canceling my pharmacy pickup right now. This post saved my life. I’m posting this to my whole family group chat. Thank you. 💀
Himanshu Singh
February 5, 2026 AT 03:28
The real tragedy isn't the medicine-it's that we've forgotten how to listen to our bodies. In ancient times, a fever was a signal. A change in urine, a strange dizziness-these were messages. Now we swallow pills to silence the message. But the body never stops screaming. We just stopped learning its language.
Jamie Hooper
February 6, 2026 AT 02:58
mate i just took ibuprofen last week for my knee. im gonna go check my eGFR now. hope i dont end up like that melbourne lady. thanks for the wake up call
Husain Atther
February 7, 2026 AT 10:25
This is a critical public health issue that requires systemic reform. The current paradigm of reactive medicine, rather than preventive pharmacovigilance, places undue burden on patients. Standardization of eGFR-based prescribing protocols across all primary care systems is not optional-it is ethically imperative.
Helen Leite
February 7, 2026 AT 18:49
I KNOW THIS IS A CONSPIRACY. They put the bad drugs in the water supply so people need more dialysis. I saw it on a video. The government and the hospitals are in cahoots. 🚨💧🩸
Izzy Hadala
February 9, 2026 AT 12:24
The data presented here aligns with current nephrological guidelines from the National Kidney Foundation's KDOQI, particularly regarding the pharmacokinetic alterations in patients with an eGFR <60 mL/min/1.73m². Further longitudinal studies are warranted to assess the efficacy of automated EHR-based drug adjustment alerts in reducing iatrogenic acute kidney injury.