Chronic Kidney Disease (CKD) Overview
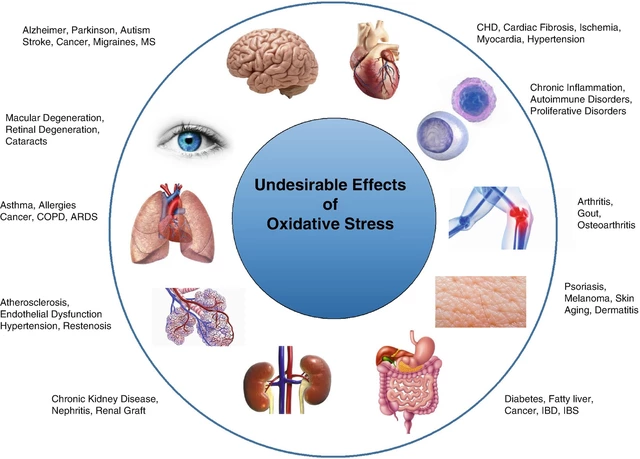
When dealing with Chronic Kidney Disease (CKD), a progressive loss of kidney function that impairs waste removal and fluid balance. Also known as renal insufficiency, it affects millions worldwide and often co‑exists with other health issues.
One key player is Hypertension, high blood pressure that speeds up kidney damage. Managing blood pressure is essential because uncontrolled CKD can lead to Cardiovascular Disease, heart failure, stroke and arterial calcification. Another frequent companion is Hyperparathyroidism, overactive parathyroid glands that cause calcium imbalance in CKD patients. Both conditions shape treatment choices, from phosphate binders to specific antihypertensive drugs.
Key considerations for CKD management
CKD demands a layered approach. First, monitor glomerular filtration rate (GFR) to gauge progression. Second, control blood pressure—ACE inhibitors or ARBs often work best. Third, address mineral‑bone disorder; vitamin D analogs and calcimimetics help curb hyperparathyroidism. Fourth, watch for cardiovascular complications; regular lipid panels and lifestyle changes are a must. Finally, when GFR falls below critical thresholds, discuss dialysis or transplant options. Below you’ll find a curated list of articles that dive into each of these topics, from drug comparisons like warfarin vs DOACs to practical guides on buying affordable generic medicines safely. These resources give you actionable steps to manage CKD and its related health challenges.