When patients leave a doctor’s office feeling unheard, confused, or rushed, it’s not always because the diagnosis was wrong. More often, it’s because the healthcare communication failed. Studies show that poor communication contributes to 80% of serious medical errors, and up to 20% of adverse outcomes are directly tied to how information is shared between providers and patients. That’s why hospitals, universities, and health systems across the U.S. are investing in structured, evidence-based education programs designed to fix this broken link.
Why Communication Training Isn’t Optional Anymore
For decades, medical training focused on technical skills: diagnosing diseases, prescribing meds, performing procedures. But communication? That was assumed. You either had it or you didn’t. Then the data came in. The Agency for Healthcare Research and Quality found that 15-20% of patient harm could be prevented with better communication. Johns Hopkins Medicine discovered physicians who completed communication training had 30% fewer malpractice claims. Press Ganey’s 2022 data showed patient satisfaction scores rose sharply-correlating at r=0.78-with how well providers listened, explained, and responded with empathy. It’s not just about being nice. It’s about safety. When a patient doesn’t understand their discharge instructions, they’re more likely to end up back in the ER. When a nurse doesn’t clearly hand off a patient’s condition during shift change, critical details get lost. And when a provider interrupts a patient after just 13.3 seconds-on average, as UCSF’s Dr. Robert Wachter documented-important symptoms go unreported. These aren’t abstract problems. They’re daily realities in clinics, hospitals, and nursing homes. That’s why institutions are no longer leaving communication to chance.What These Programs Actually Teach
Not all communication training is the same. Some are short online modules. Others are full master’s degrees. But the best ones share a common structure: they focus on specific, measurable behaviors-not vague ideas like “be more empathetic.” Take the Program for Excellence in Patient-Centered Communication (PEP) at the University of Maryland. It’s a 6.5-hour workshop accredited by the AMA. Trainees don’t just watch videos. They practice skills like “eliciting the patient’s story” and “responding with empathy” using real clinical scenarios. The goal? To help providers slow down, listen fully, and respond in ways that make patients feel seen. Mayo Clinic’s online course goes further. It uses 12 standardized patient actors to simulate tough situations: delivering bad news, setting boundaries with demanding patients, handling anger. Nurses who took it reported a 40% drop in burnout within three months-not because they worked fewer hours, but because they felt more in control of their interactions. Then there’s Northwestern University’s Mastery Learning model. Medical students must hit an 85% proficiency threshold on communication assessments before moving forward. They do 4-6 simulation sessions during clinical rotations. The result? 37% higher skill retention after six months compared to traditional lectures. These aren’t just feel-good exercises. Each skill is tied to an outcome: fewer readmissions, lower complaint rates, better adherence to treatment plans.Who These Programs Are For
You might think this is only for doctors. It’s not. The Society for Healthcare Epidemiology of America (SHEA) offers a $75-$125 course for infection preventionists and antimicrobial stewards. It teaches them how to communicate complex policies to staff, handle media inquiries, and correct misinformation on social media. One reviewer from Cleveland Clinic said a single module helped her reach 50,000 people with accurate vaccine info. The University of Texas at Austin’s Health Communication Training Series (HCTS) targets public health workers. After the pandemic exposed how slow and chaotic communication can be during crises, they built free, self-paced modules on outbreak response, risk messaging, and community trust-building. Their data showed 40% of early pandemic delays were due to poor internal or public communication. Even administrative staff are getting trained. Why? Because if the front desk doesn’t explain appointment changes clearly, or if billing staff can’t explain insurance codes in plain language, patients get frustrated-and leave. The message is clear: communication is a team sport. Every role matters.
The Real-World Impact
Numbers don’t lie. Hospitals that implemented these programs saw:- 23% higher patient satisfaction scores than those using generic training (University of Maryland, 2018)
- 28% fewer patient complaints in residency programs using mastery learning (Northwestern, 2023)
- 30% lower malpractice claims among trained physicians (Johns Hopkins, 2019)
- 73% adoption rate when clinical champions led the rollout (Northwestern, 2022)
Where These Programs Fall Short
It’s not all success stories. Many programs struggle with one big problem: sustainability. Only 12% of programs track whether skills are still being used six months after training. That’s a huge blind spot. Learning a skill is one thing. Using it daily under time pressure is another. Many clinicians say they know what to do-they just don’t have time. A 2023 AAMC survey found 58% of healthcare workers felt communication skills were important but impossible to apply during 15-minute appointments. Some programs also ignore equity. A 2023 AHRQ report found a 28% satisfaction gap between white patients and minority patients, largely due to cultural misunderstandings. Only 74% of new programs now include cultural humility training-meaning one in four still treats communication as a one-size-fits-all skill. And then there’s faculty resistance. As Northwestern’s Dr. Vineet Arora pointed out, the biggest barrier isn’t the curriculum-it’s getting teachers to learn it first. Many senior staff were never trained themselves and don’t see the value.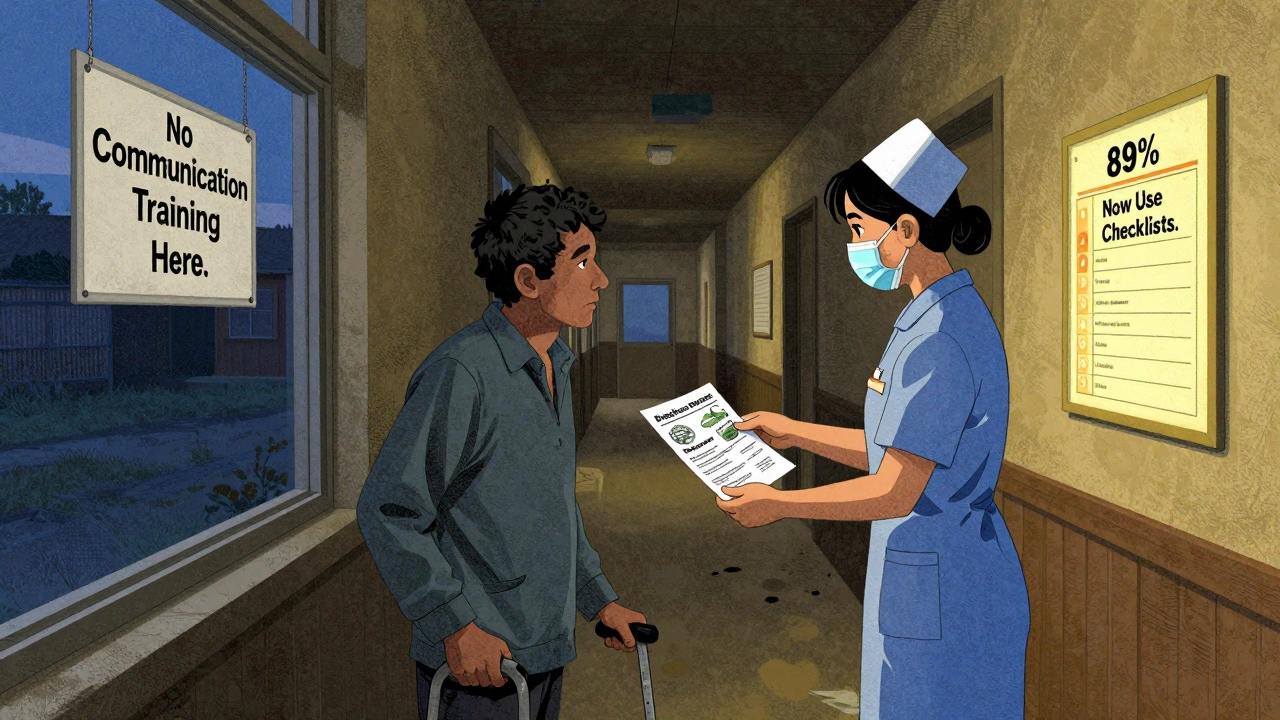
How to Make It Work
The most successful programs follow a proven four-step model from the Academy of Communication in Healthcare:- Assess the gap-Use patient surveys to find where communication breaks down. Is it discharge instructions? Pain management? Language barriers?
- Pick 3-5 high-impact behaviors-Don’t try to fix everything. Focus on what matters most.
- Train in context-Use real cases from your own clinic or hospital. No hypotheticals.
- Embed it in workflow-Add prompts in the EHR. Use checklists. Make communication part of the standard process, not an extra task.

sean whitfield
December 5, 2025 AT 05:43
So we're spending millions to teach doctors to say 'I hear you' instead of fixing the 12-minute appointment clock that's crushing everyone
Meanwhile, the real problem? Insurance companies dictate how long you can talk. Not a single program mentions that.
They train you to listen better... while the system screams at you to move on.
It's like teaching a firefighter to be polite while the building burns down.
Communication training is a Band-Aid on a hemorrhage.
And don't get me started on the EHR checklists.
They turn empathy into a checkbox.
They're not training doctors.
They're training compliance robots.
And the worst part? We're all supposed to be impressed.
Pathetic.
Carole Nkosi
December 7, 2025 AT 01:41
You think this is about communication? No.
This is about control.
They train nurses to 'listen better' so they don't complain about being overworked.
They train doctors to 'explain clearly' so patients don't sue when the system fails them.
It's not healing.
It's damage control wrapped in buzzwords.
And who pays for all this? Patients.
Through higher bills.
Through longer waits.
Through more bureaucracy.
They don't want you to be heard.
They want you to stop asking questions.
That's the real goal.
Stop pretending this is about care.
It's about profit.
Always has been.
Stephanie Bodde
December 8, 2025 AT 04:39
This made me cry in the best way 😭
Finally someone is saying what we’ve all felt.
My aunt went to the ER last month and the doctor didn’t even look up from the screen.
She left scared and confused.
But then she got trained in a hospital program last week - and now she says she actually feels like a person again.
It’s not magic.
It’s just being treated like a human.
And that? That changes everything.
Keep pushing for this. We need more of it.
Thank you for writing this.
💖
Rupa DasGupta
December 9, 2025 AT 21:07
Ugh I’m so tired of this performative woke crap
They think saying ‘I hear you’ fixes systemic collapse?
My cousin is a nurse in Texas - she works 14 hour shifts, 7 days a week, gets yelled at by patients who don’t understand their $3000 bill, and then gets told to ‘be more empathetic’ in a 20-minute Zoom module.
It’s not training.
It’s gaslighting.
And now they’re gonna make us pay for it?
And you call this progress?
Wake up.
They don’t want you to be heard.
They want you to be quiet.
And they’re selling you a fake solution so you stop screaming.
😭
Marvin Gordon
December 10, 2025 AT 05:28
Let’s be real - this is the most important thing happening in healthcare right now.
Not the new MRI machine.
Not the fancy new drug.
But the fact that someone finally said: ‘Hey, maybe if we actually talk to people, they won’t die.’
It’s not rocket science.
It’s basic human decency.
And the data proves it.
More understanding = fewer ER returns.
More listening = fewer lawsuits.
More empathy = fewer burned-out staff.
It’s not optional.
It’s the foundation.
And if your hospital doesn’t have this - demand it.
Not tomorrow.
Today.
Because lives are on the line.
And no algorithm can replace a human voice saying ‘I’m here.’
ashlie perry
December 11, 2025 AT 15:16
Did you know the CIA used similar training on interrogators in the 90s?
They called it ‘rapport building’
Same phrases.
Same scripts.
Same ‘empathy’ techniques.
Now they’re using it on cancer patients?
It’s not healing.
It’s manipulation.
They’re not teaching communication.
They’re teaching compliance engineering.
And you’re all applauding.
They’ve been doing this for decades.
They just changed the label.
From ‘interrogation’ to ‘patient-centered care’.
Same tool.
Same goal.
Same control.
Wake up.
It’s all a setup.
Stephanie Fiero
December 12, 2025 AT 21:56
OMG YES I’M A NURSE AND THIS IS SO TRUE
we had this training last year and i thought it was gonna be another boring powerpoint
but we did role plays with real patient scenarios
and i cried in the bathroom after
because i realized i hadn’t looked a patient in the eye in 3 months
and i didn’t even notice
now i start every visit with ‘what’s your biggest worry right now?’
it takes 10 seconds
but it changes everything
my patients trust me more
and i don’t feel like a robot anymore
thank you for saying this
you’re not alone 💪
Jimmy Jude
December 13, 2025 AT 12:14
Let me tell you how this really works.
They train the nurses to be ‘empathetic’ so the doctors don’t have to.
They train the receptionists to ‘explain clearly’ so the billing department doesn’t get sued.
They train the interns to ‘listen’ so the attending doesn’t have to slow down.
It’s a pyramid scheme of emotional labor.
And the people at the top? They never get trained.
They get raises.
They get vacations.
They get to say ‘we did our part’ while the frontline burns out.
This isn’t progress.
It’s exploitation with a smiley face.
And you’re all drinking the Kool-Aid.
Pathetic.
Juliet Morgan
December 14, 2025 AT 06:09
My dad’s a retired ER doc and he said the one thing that saved him after 30 years was a 30-minute workshop on ‘pausing before responding’
He used to interrupt patients at 12 seconds like everyone else
Then he learned to just… wait.
Just sit with the silence.
And guess what?
Patients told him things they’d never said before.
One woman admitted she was hiding her insulin because she couldn’t afford it.
That changed his whole approach.
It’s not about fancy scripts.
It’s about giving space.
And honestly?
That’s the hardest skill to teach.
But the most powerful.
Thank you for writing this.
I’m sharing it with my whole family.