Warfarin Interactions: What You Need to Know About Drugs, Foods, and Supplements
When you take warfarin, a blood thinner used to prevent dangerous clots. Also known as Coumadin, it works by slowing down your body’s ability to form clots—but it’s not a set-it-and-forget-it medication. Even small changes in what you eat, take, or do can throw off its balance and put you at risk. A tiny shift in your warfarin interactions can mean the difference between a clot forming and bleeding too much. That’s why understanding what affects it isn’t optional—it’s life-saving.
Many things interact with warfarin, but three stand out: other drugs, medications that change how warfarin is processed or how your blood clots, vitamin K, a nutrient that directly counteracts warfarin’s effect, and supplements, including herbal products people assume are harmless. Antibiotics like trimethoprim-sulfamethoxazole can spike your INR and cause bleeding. On the flip side, some antifungals or even common painkillers like ibuprofen can make warfarin more powerful. Vitamin K, found in leafy greens like kale and spinach, works against warfarin—so if you suddenly eat more or less of it, your INR can swing wildly. Supplements like garlic, ginkgo, or fish oil don’t come with warning labels, but they can thin your blood too, adding up to dangerous levels.
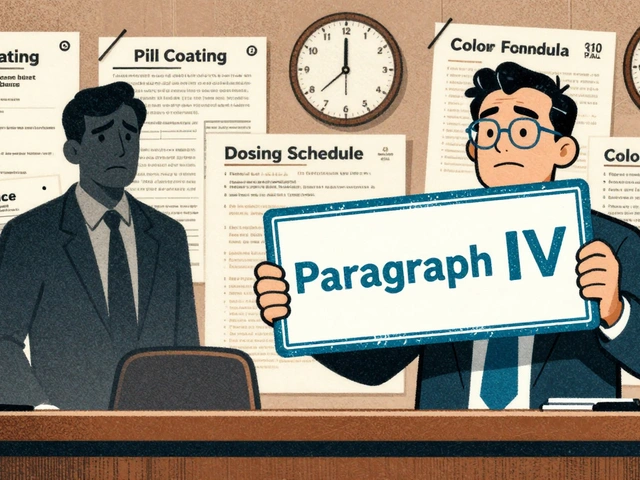
It’s not just about what you take—it’s about consistency. You don’t have to avoid spinach forever, but you need to eat about the same amount every week. The same goes for alcohol: a drink now and then is usually fine, but bingeing or going cold turkey can both mess with your levels. Your doctor doesn’t just check your INR to see if you’re "on target"—they’re watching for patterns. Did your INR jump after you started a new antibiotic? Did it drop when you switched from orange juice to grapefruit juice? Those details matter. Even something as simple as switching brands of warfarin can cause issues because different formulations absorb slightly differently.
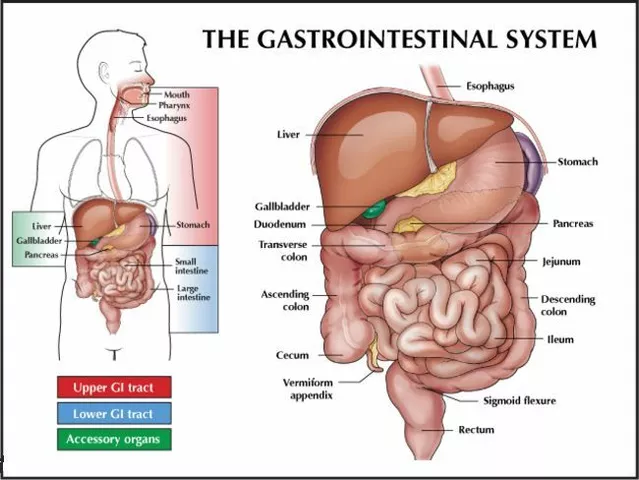
The posts below give you real-world insights into how these interactions play out. You’ll find stories from people who learned the hard way that a new supplement or a change in diet threw their INR off. You’ll see how doctors use databases to track unexpected reactions, how generic versions can behave differently, and what to ask your pharmacist before adding anything new to your routine. This isn’t theory—it’s what happens when people don’t know the rules. You don’t need to memorize every drug name. Just learn the patterns: if it affects your liver, your gut, or your blood, it might affect warfarin. And if you’re unsure? Always check. One question could prevent a hospital visit.