When your kidneys fail, life changes overnight. Dialysis keeps you alive, but it doesn’t give you back your life. For many, a kidney transplant is the only real path to freedom - from needles, schedules, and exhaustion. It’s not a cure, but it’s the closest thing. And for most people who get one, it works. Better than dialysis. Better than anything else.
Who Can Get a Kidney Transplant?
You don’t need to be young or perfect to qualify. But you do need to be well enough to survive the surgery and stick with the lifelong care that follows. The main requirement? End-stage renal disease. That means your kidneys are working at 15% or less of normal capacity. Doctors measure this with your GFR - glomerular filtration rate. If it’s below 20 mL/min, you’re typically eligible. Some centers, like Mayo Clinic, will even consider you if your GFR is up to 25 mL/min, especially if it’s dropping fast or you have a living donor lined up.Age isn’t a hard barrier. You can be 75 and still qualify if you’re otherwise healthy. Centers like UCLA don’t set an upper age limit - they look at your heart, your lungs, your strength, and your support system. The real question isn’t how old you are. It’s whether your body can handle the stress of surgery and recovery.
Obesity is a big hurdle. If your BMI is over 45, most centers won’t proceed. Some, like Vanderbilt, won’t even consider you if your BMI is above 35 without weight loss first. Why? Because extra weight makes surgery riskier. It raises the chance of infection, poor healing, and even kidney failure after transplant. Studies show obese patients have a 35% higher risk of surgical complications and a 20% higher chance of losing the new kidney.
Your heart and lungs matter just as much as your kidneys. If you have severe pulmonary hypertension - pressure in your lung arteries above 70 mm Hg - you’re not a candidate. Same goes for long-term oxygen dependence. Your heart needs to pump well too. Ejection fraction below 35%? That’s usually a stop sign. You’ll need cardiac tests - echocardiograms, stress tests, sometimes a heart catheter - before they’ll even put you on the list.
What Disqualifies You?
Some things are absolute deal-breakers. No exceptions.Active cancer. If you’re currently being treated for cancer, or if your cancer is likely to come back after transplant, you’re not eligible. Most centers require you to be cancer-free for at least two years before considering you - longer for aggressive cancers like melanoma or lung cancer.
Untreated infections. HIV isn’t automatic disqualification anymore, but only if your viral load is undetectable and your CD4 count is above 200. Same with hepatitis B - if the virus is active in your blood, you’re out. You need to be clean of active infections like tuberculosis or endocarditis before surgery.
Drug or alcohol abuse. If you’re still using street drugs or drinking heavily, you won’t get a transplant. It’s not about judgment - it’s about survival. Immunosuppressants are dangerous if you miss doses or mix them with alcohol. You’ll need to prove you’ve been clean for at least six months, often with counseling and random testing.
Severe mental illness without support? Also a no. If you’re unable to manage your own meds, attend appointments, or understand the risks, transplant centers won’t risk giving you a kidney. That’s why every center checks your mental health, your support system, and your ability to follow through. They don’t just want to save your life - they want to make sure it lasts.
The Evaluation Process
Getting on the list isn’t a quick phone call. It’s a months-long process.You’ll start with blood tests - to check your immune system, blood type, and tissue match. Then you’ll get screened for viruses like HIV, hepatitis, and CMV. A chest X-ray and EKG look at your heart and lungs. Cancer screening includes colonoscopies, mammograms, skin checks - whatever’s age-appropriate.
But the most overlooked part? Your social and emotional readiness. Penn Medicine and Vanderbilt both use frailty tests. They check your grip strength, how fast you walk, whether you’ve lost weight without trying, and if you feel exhausted most days. If you’re frail, your chances of surviving surgery drop. They’ll also ask: Who drives you to appointments? Who reminds you to take your pills? Who calls the doctor if something’s wrong?
Most centers require a care partner. Someone who’s in it for the long haul. Not just family - someone reliable. If you live alone and have no one, you’ll be asked to find someone before they’ll list you. It’s not cruel. It’s practical. You’ll need help for months, maybe years.
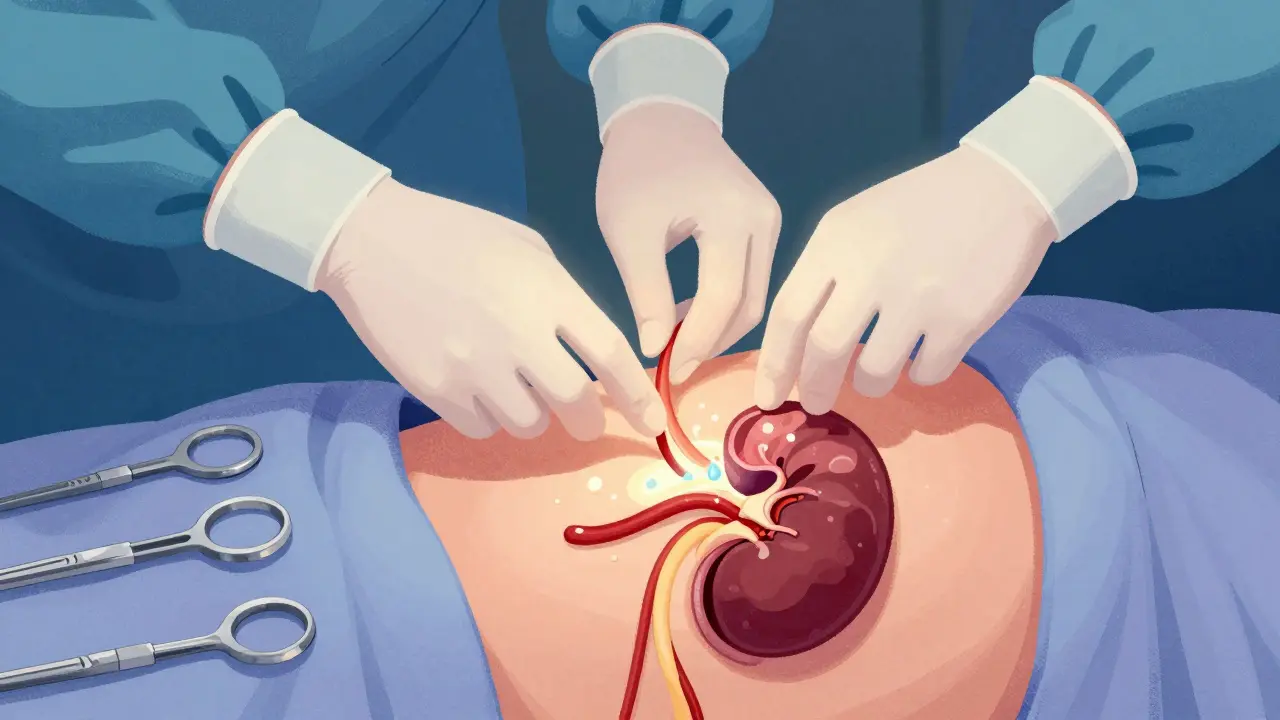
The Surgery
The operation itself takes about three to four hours. You’re under full anesthesia. The surgeon places the new kidney in your lower belly - usually on the right or left side. The blood vessels of the new kidney are stitched to your own arteries and veins. The ureter - the tube that carries urine - is connected to your bladder.Here’s something people don’t expect: your old kidneys usually stay in. Unless they’re infected, causing high blood pressure, or bleeding, they’re left alone. The new kidney doesn’t need them out of the way.
When blood starts flowing into the new kidney, you might see it make urine right away. That’s a good sign. But sometimes, it takes days. About 20% of deceased donor kidneys don’t start working immediately. That’s called delayed graft function. You’ll need dialysis for a few days until it kicks in. It’s not failure. It’s normal.
Recovery in the hospital takes about three to five days. You’ll be up walking the next day. Pain is managed, but you’ll feel sore. You’ll be on antibiotics and antivirals to prevent infection. And you’ll start immunosuppressants - right away.
Life After the Transplant
This is where most people fail. Not because the surgery didn’t work. But because they stop taking their pills.You’ll need lifelong immunosuppressants. That means drugs that stop your immune system from attacking the new kidney. The standard combo? A calcineurin inhibitor like tacrolimus, an antiproliferative like mycophenolate, and a steroid like prednisone. Some centers add a monoclonal antibody at the start to prevent early rejection.
These drugs aren’t optional. Miss one dose, and your body might start rejecting the kidney. Rejection can happen anytime - even years later. That’s why you’ll see your transplant team often. Weekly for the first month. Then monthly for six months. Then every three months. Forever.
You’ll also need regular blood tests. To check your kidney function. To make sure your drug levels are right. Too little - risk of rejection. Too much - risk of infection, cancer, or kidney damage. It’s a tightrope.
Side effects are real. Weight gain. High blood pressure. Diabetes. Bone thinning. Higher risk of skin cancer. You’ll need to watch your diet, exercise, and sun exposure. No more tanning beds. No more skipping sunscreen.
But here’s the upside: your quality of life skyrockets. Most people go back to work. Travel. Play with their grandkids. Sleep through the night. No more dialysis machines. No more fluid limits. No more endless fatigue.

Success Rates and New Hope
The numbers are good. For living donor transplants, 97% of kidneys are still working after one year. For deceased donors, it’s 93%. After five years, 85% of living donor kidneys are still going strong. Deceased donor kidneys? Around 78%.There’s new hope on the horizon. The Kidney Donor Profile Index (KDPI) helps match kidneys better. A high-KDPI kidney - from an older donor or someone with health issues - used to be seen as a last resort. Now we know: even those kidneys give people years of better life than dialysis. They’re not perfect, but they’re better than nothing.
Researchers are working on tolerance protocols. The dream? Teach the immune system to accept the new kidney without lifelong drugs. Early trials at Stanford and the University of Minnesota are showing promise. In five to ten years, we might see patients off immunosuppressants entirely.
Living donation is still the gold standard. One healthy person can give a kidney and live a full, normal life. It’s not risky - the donor’s remaining kidney grows to compensate. And the recipient gets a better-functioning kidney faster.
What If It Fails?
Sometimes, the kidney doesn’t last. Rejection, infection, or scarring can cause it to fail. If that happens, you go back to dialysis. And you can be listed again for another transplant.Many people get a second - even a third - transplant. Success rates drop a little with each one, but they’re still better than staying on dialysis. The key? Stay healthy. Stay on your meds. Stay in touch with your team.
Can I get a kidney transplant if I’m over 70?
Yes. There’s no strict age limit. Centers like UCLA evaluate older patients based on overall health, heart and lung function, frailty, and support systems - not age alone. If you’re active, mentally clear, and have someone to help you manage care, you can qualify.
How long do kidney transplants last?
On average, a kidney from a living donor lasts 15-20 years. A deceased donor kidney lasts 10-15 years. Some last longer - even 30 years. But many fail earlier due to rejection, infection, or side effects of medications. Regular check-ups and strict medication adherence are the best ways to make it last.
Can I drink alcohol after a kidney transplant?
Moderation is allowed, but heavy drinking is dangerous. Alcohol can damage your new kidney and interact with immunosuppressants, increasing the risk of liver damage and rejection. Most centers recommend no more than one drink per day - and only if your liver is healthy and your doctor approves.
Do I need to change my diet after a transplant?
Yes. You’ll need to eat less salt, less sugar, and less processed food. Steroids can raise your blood sugar and cholesterol, so you’ll need to watch carbs and fats. Protein intake should be moderate - too much can strain the kidney. Your dietitian will give you a personalized plan based on your medications and lab results.
Can I get pregnant after a kidney transplant?
Yes, but only after your kidney function is stable and your medications are adjusted. Most doctors recommend waiting at least one year after transplant. Some immunosuppressants are safe during pregnancy; others aren’t. You’ll need close monitoring by both a transplant team and an obstetrician. Many women have healthy pregnancies after transplant - but it’s high-risk and requires planning.
Next Steps
If you’re considering a transplant, start by talking to your nephrologist. Ask for a referral to a transplant center. Don’t wait until you’re on dialysis. The earlier you’re evaluated, the better your chances of getting a living donor and avoiding long waits.If you’re healthy enough, consider becoming a living donor. One kidney can give someone back their life. And you’ll live just fine with one.
Transplant isn’t the end of the journey. It’s the beginning of a new one - with rules, risks, and responsibilities. But for most, it’s worth it. You get your life back. And that’s more than medicine can usually promise.

Jennifer Glass
January 4, 2026 AT 08:20
It’s wild how much we take kidneys for granted until they’re failing. I never thought about how much of your identity gets tied up in dialysis schedules-like your whole life becomes a series of appointments and fluid restrictions. A transplant doesn’t just replace an organ; it gives you back the ability to just… live. No alarms, no IVs, no wondering if you’ll make it to the next session.
And honestly? The emotional toll of waiting is worse than the surgery. You’re stuck in limbo-hoping, praying, watching your body decline while others get priority. It’s not just medical. It’s existential.
melissa cucic
January 4, 2026 AT 18:37
It's worth noting, however, that while the success rates are indeed impressive-especially for living-donor transplants-the long-term burden of immunosuppression cannot be understated. We are asking patients to live with a chronic, lifelong pharmacological intervention that carries significant risks: malignancy, renal toxicity, metabolic syndrome, and opportunistic infections. The trade-off is undeniable, but we must be transparent: this is not a cure. It is a managed condition-with a better quality of life, yes-but still, a condition.
saurabh singh
January 5, 2026 AT 02:07
Bro, I had a cousin in Delhi get a kidney from his brother-no big hospital, no fancy tech, just love and a doctor who knew his stuff. They didn’t have KDPI scores or fancy blood tests, but they had each other. And guess what? His kidney’s been working 8 years now. Sometimes the best medicine isn’t in the lab-it’s in the family.
Stop making this so clinical. People aren’t data points. They’re humans with hearts, and sometimes, they just need someone to say, ‘I’ve got you.’
Peyton Feuer
January 5, 2026 AT 17:09
wait so if you’re obese but you’re trying to lose weight can you still get on the list? i thought you had to hit a certain bmi first but maybe i’m mixing it up with bariatric surgery…
also why do they care if you have a care partner? like… what if you’re just really good at managing yourself? i’m single and i’ve got my meds on my phone and everything…
Jay Tejada
January 6, 2026 AT 00:36
They say ‘no alcohol’ but then you see people on transplant forums sipping wine like it’s a Sunday brunch. Meanwhile, I’m still waiting for my name to come up and I’ve been sober for 18 months. Guess I’m not ‘motivated enough.’
Allen Ye
January 7, 2026 AT 05:36
There’s a deeper philosophical layer here that rarely gets discussed: the transplant system forces us to confront mortality not as an abstract concept, but as a logistical problem. Who gets a kidney? Who doesn’t? Who’s deemed ‘worthy’ of a second chance? The answer isn’t medical-it’s social. It’s about who has insurance, who has family, who can navigate bureaucracy, who can prove they’re ‘compliant.’ We’ve turned life-saving care into a meritocracy of discipline. And that’s not justice. That’s privilege dressed in white coats.
And yet, we still cling to the myth that if you just try hard enough, you’ll get your kidney. The truth? Some people are just born on the wrong side of the algorithm.
mark etang
January 8, 2026 AT 22:39
It is imperative that prospective transplant recipients understand the gravity of their post-operative responsibilities. The administration of immunosuppressive regimens must be executed with unwavering precision, as deviations-however minor-may precipitate irreversible graft failure. Furthermore, adherence to scheduled laboratory monitoring is not merely recommended; it is a non-negotiable component of long-term survival. Failure to comply constitutes a breach of the implicit social contract between the donor, the medical team, and the recipient.
josh plum
January 10, 2026 AT 12:38
They let people with HIV get transplants now? Cool. So next they’ll give kidneys to drug addicts who just got out of jail. And then to people who won’t wear masks. And then to people who don’t vaccinate their kids. This isn’t medicine anymore-it’s a reward system for bad choices. Someone’s kidney is going to waste on someone who doesn’t deserve it. And guess what? The donor’s family didn’t sign up for this.
John Ross
January 12, 2026 AT 10:05
The KDPI metric is fundamentally flawed. It’s a proxy for donor quality, but it conflates biological age with physiological resilience. A 70-year-old donor with no comorbidities and a GFR of 80 mL/min is biologically superior to a 35-year-old donor with undiagnosed hypertension and microalbuminuria. We need a dynamic, multi-parametric donor risk index-not a crude age-based heuristic. And while we’re at it, let’s stop calling deceased donor kidneys ‘suboptimal.’ They’re not. They’re underutilized.
Clint Moser
January 13, 2026 AT 06:55
did you know the gov’t is secretly harvesting kidneys from people who die in car crashes? they don’t tell you that. and the drugs? they’re laced with nanobots that track your immune system. that’s why you gotta take them at exactly 7:13am or the machine gets confused. my cousin’s neighbor’s dog got a transplant and now it barks in binary. i’m not joking. check the papers. it’s all covered up.
Brendan F. Cochran
January 14, 2026 AT 19:27
Why do we even let foreigners get transplants here? We’ve got Americans waiting for years. My uncle died waiting. And now some guy from India gets one because he ‘has a care partner’? Screw that. First come, first served. American kidneys for American citizens. That’s how it should be. And if you’re overweight or on welfare? No. No. No. You don’t get to take someone else’s chance.
Mandy Kowitz
January 15, 2026 AT 03:59
Wow. So if you’re poor, old, fat, or lazy-you’re just out of luck? That’s the whole article. Just say ‘if you’re not perfect, die quietly.’
Michael Rudge
January 17, 2026 AT 01:08
It’s so cute how people think ‘having a care partner’ is the solution. Like, what, your 80-year-old mother is going to remember your tacrolimus schedule? Or your ex who ‘helps’ you but never shows up? This system isn’t designed for people-it’s designed for people who already have privilege. You think the guy with no family, no car, and a part-time job gets evaluated the same way as the CEO with a private nurse? Please.
Ethan Purser
January 17, 2026 AT 16:49
I’ve been waiting for 7 years. My wife left me because I was ‘too much.’ My kids don’t call. I cried in the parking lot after my 100th blood test. I’m not asking for a miracle. I just want someone to tell me it’s not my fault that I’m not ‘ideal.’
And then I read this article and it feels like they’re listing all the reasons I don’t deserve to live. Like I’m a burden. Like my life isn’t worth the cost of one kidney.
So I’m writing this. Not for you. For the person who’s still waiting. You’re not broken. You’re not a statistic. You’re still here. And that’s more than most people can say.