Sterile Medication Shortages: What's Behind the Gaps in Critical Drugs
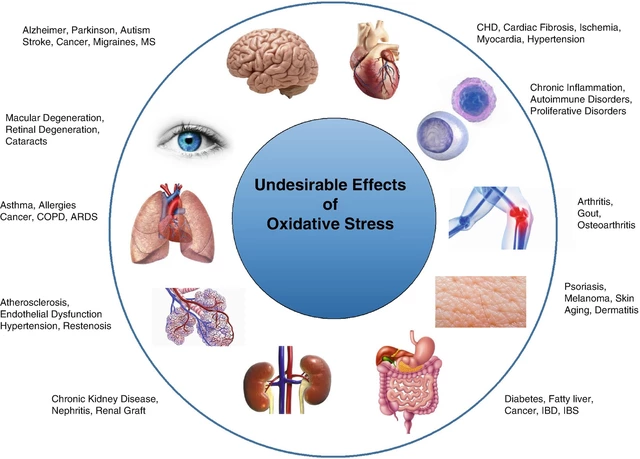
When a hospital runs out of sterile medication, injectable drugs like antibiotics, painkillers, or chemotherapy agents that must be free of contaminants, it’s not just an inventory problem—it’s a patient safety crisis. These aren’t over-the-counter pills you can swap out. Sterile medications are given directly into veins, muscles, or spinal fluid. One shortage can delay cancer treatment, increase infection risk, or force doctors to use less effective alternatives. The IV drug shortages, a subset of sterile medication gaps affecting intravenous solutions and injectables have been worsening for over a decade, with over 300 drugs on the FDA’s list at their peak. It’s not random. It’s systemic.
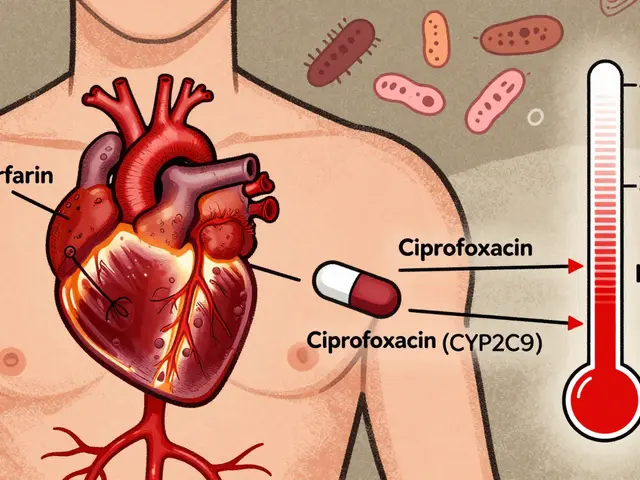
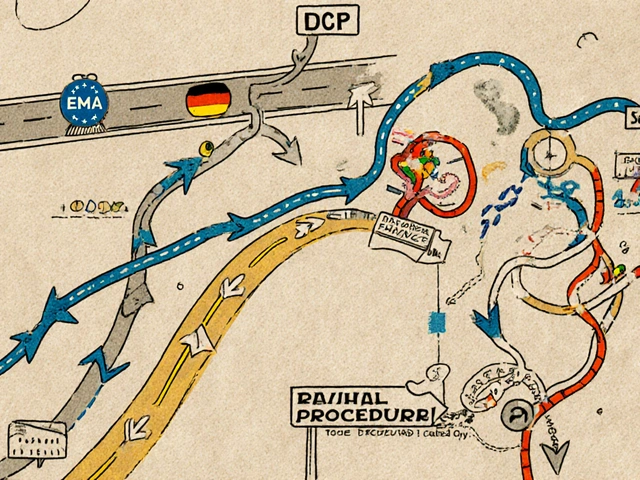
Behind every shortage is a broken medication supply chain, the network of manufacturers, distributors, and regulators that move sterile drugs from lab to bedside. Most sterile meds are made by just one or two factories, often overseas. If one plant has a quality issue—like mold in a cleanroom or a faulty sterilization process—the whole country can go dry. The sterile compounding, the process of preparing sterile drugs in pharmacies under strict controls can’t fill the gap fast enough. Hospitals can’t just mix their own vancomycin or heparin safely without specialized labs, training, and equipment. Even when alternatives exist, they may not be approved for the same use, or worse, they come with new side effects. A shortage of sterile saline? That affects everything from flushing IV lines to diluting chemo. A shortage of propofol? Surgery gets canceled. A shortage of epinephrine for anaphylaxis? Lives are on the line.
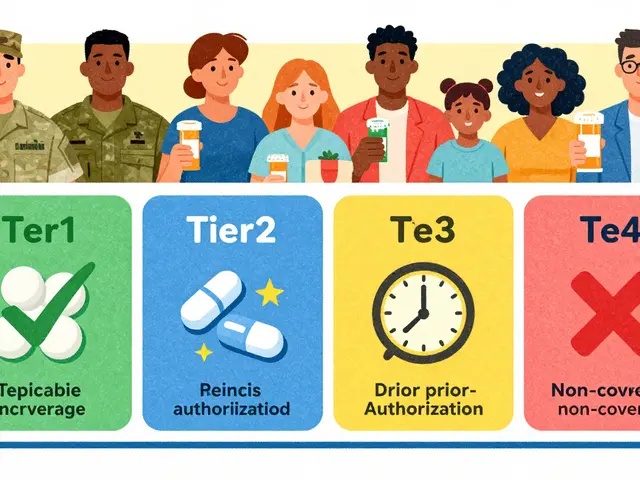
What’s worse, these shortages hit hardest where care is most urgent: ICUs, oncology units, emergency rooms. Nurses scramble to find substitutes. Pharmacists spend hours tracking down small batches. Doctors make tough calls under pressure. And patients? They’re the ones waiting longer, getting less effective treatment, or facing avoidable complications. The problem isn’t getting better. Manufacturing delays, raw material shortages, and consolidation in the pharma industry keep pushing more drugs onto the shortage list. But there’s movement. New federal rules are starting to require manufacturers to report potential shortages earlier. Some hospitals are building emergency stockpiles. Others are partnering with compounding pharmacies under strict oversight. You won’t fix this overnight—but you can understand it. Below, you’ll find real-world stories and practical insights from providers who’ve lived through these gaps. From how to spot early warning signs to what alternatives actually work, this collection gives you the facts you need to navigate the chaos.