Parkinson's disease: practical guide to symptoms, treatment and daily life
Parkinson's disease affects movement, mood and thinking in different ways for each person. If you or someone you know is getting slow, shaky, or unsteady, this guide explains what to watch for and what actually helps. I'll keep it plain and useful — no jargon.
Symptoms & diagnosis
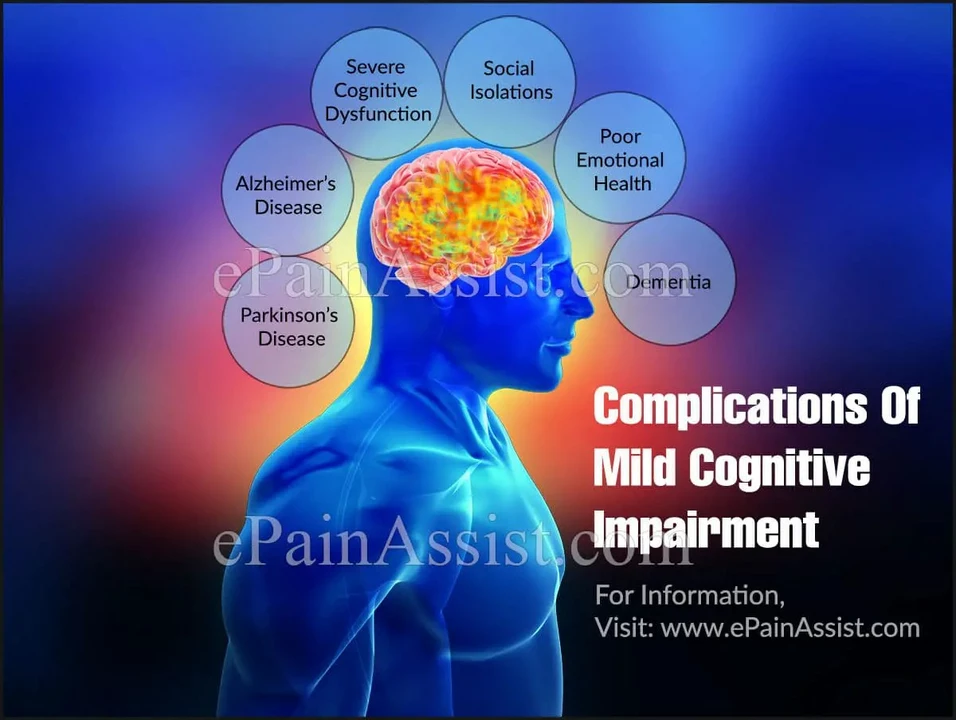
Common signs include a resting tremor (usually one hand), slowness of movement (bradykinesia), stiffness in arms or legs, and balance problems that get worse over time. Non-motor symptoms matter too: sleep changes, reduced smell, constipation, low mood and thinking changes can show up years before movement issues. Not every symptom means Parkinson's, but a pattern of several is a red flag.
Diagnosis is mostly clinical: a doctor checks history, watches how you move, and looks for a clear response to Parkinson's medicines. Imaging like DAT scans sometimes helps when the picture is unclear, but they don't replace a doctor’s exam. Getting assessed by a neurologist, ideally one with Parkinson's experience, makes a big difference for treatment plans.
Treatment and daily tips
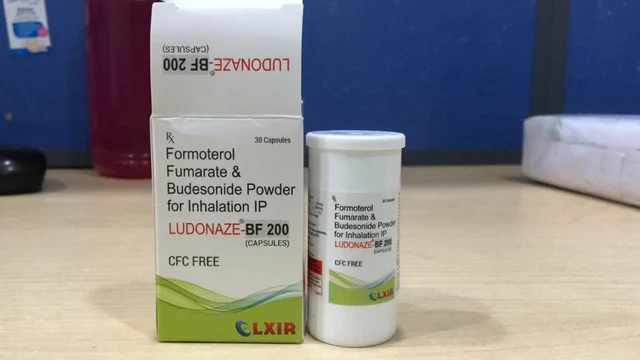
Medicine is the main tool. Levodopa remains the most effective drug for controlling movement problems. Dopamine agonists, MAO-B inhibitors and COMT inhibitors are other options doctors use to fine-tune control and reduce side effects. Deep brain stimulation (DBS) surgery helps some people when medications stop working well. Ask your specialist about pros and cons — each option carries real benefits and risks.
Daily living tips make life easier. Physical therapy focused on gait and balance helps reduce falls and keeps you active. Speech therapy can help with soft voice or swallowing issues. Regular exercise — walking, cycling or tai chi — protects mobility and mood. Small home changes, like removing rugs and improving lighting, reduce trip risks. Keep pillboxes, alarms, or apps to manage complex med schedules.
Medication safety matters, especially if you shop online. Buy from verified pharmacies, keep prescriptions current, and never mix meds without checking with your doctor or pharmacist. Some over-the-counter drugs and supplements can interfere with Parkinson's treatments — always check first.
Care and planning count. Early conversations about driving, work, and finances reduce stress later. Support groups and local Parkinson's foundations connect you with practical tips, therapy programs and clinical trial options. Family education helps everyone handle daily challenges without blame.
When to see help right away: sudden worsening of movement, new severe confusion, fainting, high fever or swallowing trouble. These are signs to call emergency services.
Every case is different. Keep a simple symptom diary to track what helps and what doesn't, bring it to appointments, and be honest about side effects. With the right team, clear information and small daily habits, people with Parkinson's often keep a good quality of life for many years.
If you want practical next steps: list your top three daily problems, bring a current meds list to every appointment, and ask about rehab referrals. If you’re a caregiver, learn safe transfer techniques and build an emergency plan. Check national Parkinson's foundation sites for reliable info and local groups for classes and meetups. Clinical trials can offer new options—ask your neurologist.