G6PD Medication Safety Checker
Check Medication Safety
Enter a medication name to see if it's safe for people with G6PD deficiency. Includes both common brand names and generic drugs.
Enter a medication name to check its safety for G6PD deficiency.
Common Medications
Acetaminophen (Tylenol)
Safe at standard doses. No oxidative stress to red blood cells.
Primaquine
High risk for hemolysis. Class I and II variants have 100% hemolysis risk at standard doses.
Methylene blue
95% of G6PD-deficient patients have severe hemolysis after a single dose.
Atovaquone-proguanil (Malarone)
Safe for G6PD-deficient people. 95% effective for malaria prevention.
Imagine taking a common medicine for an infection, only to have your red blood cells start breaking down within hours. For someone with G6PD deficiency, this isn’t a hypothetical scenario-it’s a real, life-threatening risk. Glucose-6-Phosphate Dehydrogenase (G6PD) deficiency affects around 400 million people worldwide, and most don’t even know they have it until they’re exposed to a trigger. The good news? Hemolysis isn’t random. It’s preventable. The key is knowing which medications to avoid and getting tested before taking anything new.
What G6PD Deficiency Actually Does
G6PD is an enzyme your red blood cells need to fight off oxidative damage. Think of it like a shield. When you take certain drugs, smoke, eat fava beans, or get an infection, your body produces reactive molecules that can tear up red blood cells. Normally, G6PD helps neutralize those molecules. But if you’re deficient, your shield is weak or missing. Without it, red blood cells burst open-this is hemolysis. Hemoglobin can drop from normal levels (14 g/dL) to below 7 g/dL in less than a week. That’s not just fatigue-it’s organ stress, kidney damage, and possible death if not treated fast.The condition is inherited, carried on the X chromosome. That’s why it’s more common in males, but about 15% of females with the gene can still have symptoms because of how X-chromosome inactivation works. It’s not rare. In parts of Africa, one in five people carries the gene. In the Mediterranean and Southeast Asia, rates are similar. And it’s not just a childhood issue-it lasts your whole life.
Medications That Can Trigger Hemolysis
There are 87 medications currently flagged by the WHO as dangerous for people with G6PD deficiency. But you don’t need to memorize them all. Focus on the big ones that cause the most harm:- Rasburicase-Used to treat tumor lysis syndrome. This drug generates hydrogen peroxide. In G6PD-deficient patients, it causes near-universal hemolysis. The FDA issued a Black Box Warning in January 2023. Never give it without testing first.
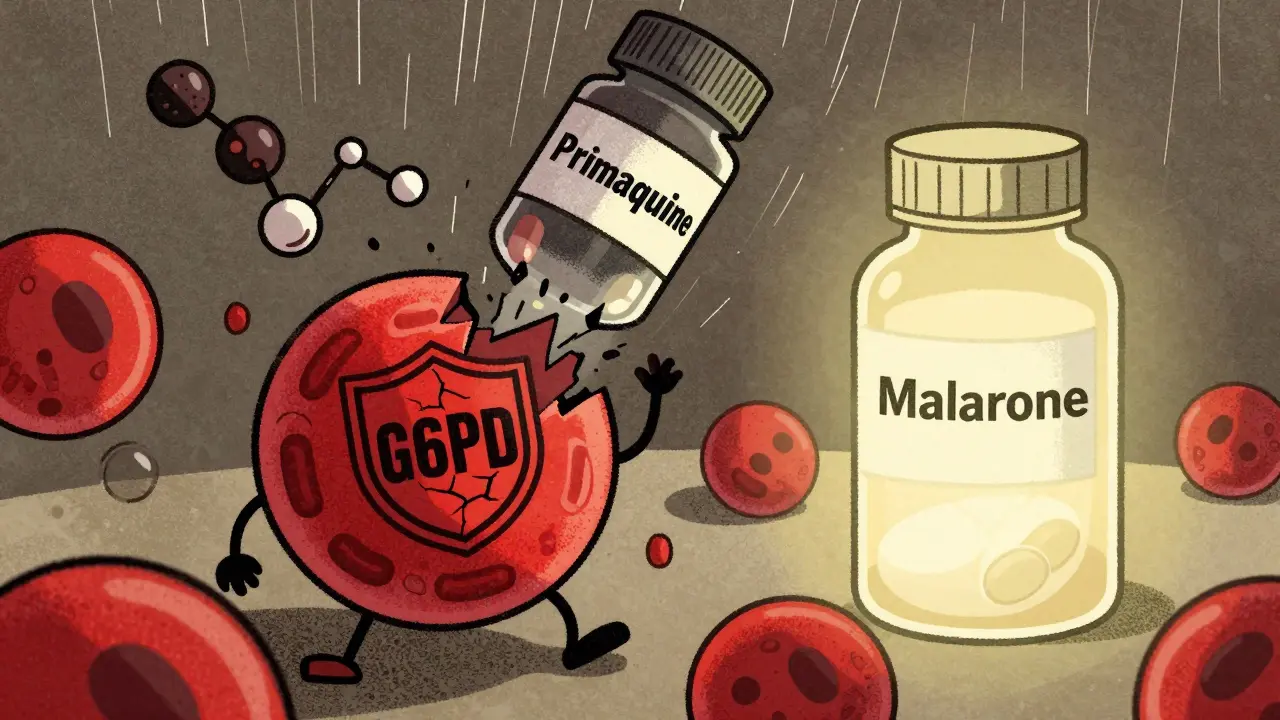
- Methylene blue-Used for methemoglobinemia. It’s ironic: the treatment for one blood problem can cause another. Studies show 95% of G6PD-deficient patients have severe hemolysis after a single dose. In one case, a patient’s hemoglobin dropped from 14.2 to 5.8 in 48 hours.
- Primaquine-A malaria drug. For decades, it was the go-to for killing dormant liver parasites. But it’s extremely risky. Class I and II G6PD variants have 100% hemolysis risk at standard doses. WHO now requires testing before use.
- Dapsone-Used for leprosy and some skin conditions. Above 50mg daily, it causes hemolysis in 80% of deficient patients. Even lower doses can be dangerous in sensitive individuals.
- Sulfonamides-Including trimethoprim-sulfamethoxazole (Bactrim). While not all sulfonamides are equally dangerous, the risk is high enough that many clinicians avoid them entirely in known cases.
Some drugs have vague warnings on their labels. For example, sulfonylureas like glyburide (used for diabetes) carry G6PD precautions in 92% of global package inserts-but only 17 documented cases exist since 1965. Experts say these warnings are often based on fear, not evidence. Still, when in doubt, avoid.
Safe Alternatives
You don’t have to go without treatment. Safe options exist for nearly every condition:- Malaria prevention: Use atovaquone-proguanil (Malarone) instead of primaquine. For travelers, it’s 95% effective and completely safe for G6PD-deficient people.
- Malaria treatment: Artemisinin-based combination therapies (ACTs) are safe in all G6PD classes. Tafenoquine is now approved-but only if you’ve had a quantitative G6PD test confirming you’re not severely deficient.
- Methemoglobinemia: Use ascorbic acid (vitamin C) instead of methylene blue. It’s slower, but safe. In emergencies, exchange transfusion may be needed.
- Infections: Most antibiotics like amoxicillin, cephalexin, and azithromycin are safe. Avoid sulfa drugs unless no alternatives exist.
- Pain relief: Acetaminophen (paracetamol) is fine. Avoid high-dose aspirin and NSAIDs like naproxen in acute hemolytic episodes.
Testing: When and How
The biggest problem? Most people aren’t tested until after they’re already sick. That’s too late. The best time to test is before any new medication is given-or better yet, at birth.Point-of-care tests now exist that give results in under 15 minutes. The STANDARD G6PD Test System, approved by the FDA in January 2024, delivers 99.1% accuracy in just eight minutes. In emergency rooms, this can prevent deadly mistakes. In newborn screening programs, it’s saved lives. Saudi Arabia reduced hemolytic crisis admissions by 78% after implementing universal newborn testing.
But here’s the catch: you can’t test right after a hemolytic episode. Your body is still rebuilding red blood cells. The new ones have normal enzyme levels, so the test will falsely look normal. Wait at least three months after the last crisis for an accurate result.
Quantitative testing is essential. Fluorescent spot tests are good for screening, but they don’t tell you how severe your deficiency is. Class II (Mediterranean variant) patients need stricter avoidance than Class III (common African variant). Genetic testing can identify your exact mutation, but it’s expensive and not always necessary if you’re avoiding triggers.
What to Do If You’re Diagnosed
If you or your child has been diagnosed:- Get a medical alert bracelet. It should say “G6PD DEFICIENT-AVOID OXIDATIVE DRUGS.”
- Keep a printed list of unsafe medications. Update it yearly. The WHO and NIH have free downloadable lists.
- Teach your family and caregivers. A nurse in Texas gave methylene blue to a G6PD-deficient patient because no one knew the risk. He needed three blood transfusions.
- Carry a copy of your test results. Many doctors don’t know G6PD details. Be your own advocate.
- Ask before taking any new drug-even over-the-counter ones. Herbal supplements like naphthalene (mothballs) and vitamin K analogs can also trigger hemolysis.
One study found that 92% of patients who received full education on triggers had zero hemolytic episodes over five years. Those who didn’t? Only 38% stayed safe. Knowledge isn’t just helpful-it’s lifesaving.

Global Gaps and Progress
You’d think this would be standard care by now. But only 18 of 47 African countries have national G6PD screening programs. In the U.S., only 12 states require newborn testing, even though 1 in 10 African American males has the condition. The Global Fund has invested $127 million to fix this in malaria zones. The WHO now lists G6PD testing as essential for safe malaria treatment.Research is moving fast. A 2024 study showed N-acetylcysteine (NAC) can protect red blood cells from oxidative damage when given with primaquine. That could open the door to safer malaria treatment for millions. Phase I trials for enzyme replacement therapy start in late 2024. In the future, we might be able to fix the enzyme itself.
Right now, though, prevention is still the only proven method. No surgery. No long-term drugs. Just awareness and avoidance.
Final Advice
If you’re from a region with high G6PD prevalence-Africa, the Mediterranean, Southeast Asia-or if you have family members with unexplained anemia, get tested. Don’t wait for a crisis. If you’re prescribed a new medication, ask: “Is this safe for someone with G6PD deficiency?” If the answer isn’t clear, get a second opinion. For every person who dies from a preventable hemolytic episode, there are dozens more who suffer, are hospitalized, or lose weeks of work.The tools to prevent this are here. The science is solid. The question isn’t whether we can stop it. It’s whether we will.
Can G6PD deficiency be cured?
No, G6PD deficiency is a genetic condition and cannot be cured. But it can be managed effectively by avoiding oxidative triggers like certain medications, fava beans, and infections. With proper precautions, most people live normal, healthy lives without complications.
Is G6PD deficiency only a problem for men?
No. While the gene is on the X chromosome and males are more commonly affected, about 15% of females who carry the gene can still experience hemolysis. This happens due to X-chromosome inactivation, where some of their red blood cells turn off the healthy gene. Women should not assume they’re safe just because they’re female.
Can I take acetaminophen (Tylenol) if I have G6PD deficiency?
Yes. Acetaminophen is considered safe for people with G6PD deficiency at standard doses. It does not cause oxidative stress to red blood cells. Avoid high doses or prolonged use without medical advice, but normal use for pain or fever is not a risk.
What should I do if I accidentally take a dangerous medication?
Stop taking the medication immediately and seek medical help. Symptoms of hemolysis include dark urine, yellowing skin, extreme fatigue, shortness of breath, and rapid heartbeat. Blood tests will check hemoglobin and bilirubin levels. Treatment may include fluids, oxygen, and in severe cases, blood transfusions. Early intervention prevents kidney damage and death.
Can I get tested for G6PD deficiency before taking a new drug?
Yes, and you should. Many hospitals and clinics now offer rapid G6PD tests that give results in under 15 minutes. If you’re from a high-prevalence region, have a family history, or are about to take a drug like primaquine or methylene blue, insist on testing. Waiting until after a reaction is dangerous and avoidable.
Are herbal supplements safe for G6PD deficiency?
Many are not. Avoid supplements containing naphthalene (found in mothballs), high-dose vitamin K, and certain traditional remedies like kava or aristolochic acid. Even natural doesn’t mean safe. Always check with a doctor before taking any herbal product if you have G6PD deficiency.
Liam Tanner
January 2, 2026 AT 13:56
Just had my kid tested after a scary episode with Bactrim. Turned out he’s Class III deficiency. We’re now keeping the WHO list on the fridge next to the insulin. Knowledge really is power.
Palesa Makuru
January 3, 2026 AT 13:01
Oh please. Another ‘educational’ post from someone who read a WHO pdf and thinks they’re a hematologist now. Most of these ‘avoid’ lists are outdated fear-mongering. I’ve been G6PD deficient since birth, never had an issue with sulfa drugs, and I live in Johannesburg where half the population has this. Stop scaring people with half-baked guidelines.
Sarah Little
January 3, 2026 AT 14:05
While the clinical guidelines are robust, the translational gap in primary care remains significant. The sensitivity of point-of-care assays like the STANDARD G6PD Test System is excellent, but in resource-limited settings, pre-analytical variables-like hemolysis timing, RBC turnover kinetics, and assay calibration-can introduce false negatives. We need standardized protocols, not just tools.
innocent massawe
January 3, 2026 AT 22:23
God bless this post. 🙏 I'm from Nigeria, and my cousin died at 12 because they gave him sulfa for fever. No one knew. I carry the list on my phone now. Please, if you're from Africa or Asia-get tested. It's not about fear. It's about living.
Ian Ring
January 4, 2026 AT 12:48
Thank you. Finally, someone who gets it. I’m a GP in Manchester, and I’ve seen two near-fatal cases in the last year. One was a 4-year-old given methylene blue for ‘cyanosis’-no testing. The other was a veteran on dapsone for psoriasis. Both survived, but barely. This isn’t theoretical. It’s happening in our clinics.
Shanahan Crowell
January 5, 2026 AT 19:16
If you’re reading this and you’re from a high-prevalence area-DO NOT WAIT. Get tested. Your life isn’t a gamble. The test takes 8 minutes. The consequences of ignoring it? Weeks in ICU. Don’t be the person who says, ‘I didn’t know.’ You know now. Act.
Kerry Howarth
January 6, 2026 AT 16:55
Acetaminophen is safe. Aspirin isn’t. Malarone is safe. Primaquine isn’t. Test before you take anything new. That’s it.
Joy F
January 7, 2026 AT 23:10
Let’s be real: this isn’t about medicine. It’s about systemic neglect. Why are we still relying on patient self-advocacy in 2025? Why isn’t G6PD screening as routine as hearing tests for newborns? Because it’s cheaper to let people die quietly in rural clinics than fund universal testing. This is medical apartheid wrapped in a ‘precautionary principle’.
And don’t even get me started on the pharmaceutical industry’s silence. They profit from treating the complications they helped create. Rasburicase? Black Box Warning. But still pushed in oncology wards. Why? Because no one’s suing them yet.
And the herbal supplement warning? Of course it’s ignored. People trust ‘natural’ more than FDA. That’s not ignorance-it’s capitalism. They sell you mothballs as ‘detox’ and call it wellness. We’re not just failing patients-we’re failing ethics.
And yet, here we are, in 2025, still having this conversation. Like it’s new. Like it’s not documented since the 1950s. Wake up. This isn’t a medical footnote. It’s a human rights issue.
Haley Parizo
January 9, 2026 AT 08:25
There’s a deeper truth here: we treat genetic conditions like moral failures. ‘Why didn’t you get tested?’ as if it’s your fault you were born with a broken shield. But G6PD deficiency isn’t a flaw-it’s an evolutionary adaptation. It protected millions from malaria. We’re the ones who’ve broken the balance by overprescribing. We’re the ones who need to change-not the people carrying this gene.
And yet, we still label them ‘at-risk.’ Like they’re broken. Like they’re the problem. We should be calling these drugs ‘dangerous for populations with evolutionary adaptations.’ That’s the real diagnosis.
It’s not about avoiding drugs. It’s about evolving our medicine to respect biology-not force conformity.
Ian Detrick
January 9, 2026 AT 15:00
One thing people don’t talk about: the psychological toll. I’ve had patients who refuse to take any new meds-even Tylenol-because they’re terrified. They’re not paranoid. They’ve seen friends die. We need better education, but we also need compassion. This isn’t just clinical. It’s emotional trauma passed down through families.
Angela Fisher
January 9, 2026 AT 16:46
Wait… so you’re telling me the government knows about this but doesn’t test everyone? And Big Pharma is hiding this? And they’re pushing methylene blue anyway? And your doctor doesn’t even know? And the WHO just says ‘test’ but doesn’t fund it? And they’re using ‘natural remedies’ that are actually poison? This is a cover-up. I’ve been reading forums-people are dying in silence. They’re calling it ‘mysterious anemia.’ It’s not mysterious. It’s murder by negligence. Someone’s getting paid to keep this quiet. I’m not crazy. I’ve seen the emails. The FDA has internal memos. They’re waiting for the lawsuits. Don’t trust anyone. Get your DNA tested. Now.
Neela Sharma
January 9, 2026 AT 18:59
My aunt in Mumbai died from a simple antibiotic-she never knew. Now I carry a little card in my purse: ‘G6PD Deficient.’ I give it to pharmacists. Sometimes they laugh. Sometimes they cry. Either way, they remember. One pharmacist in Delhi now prints these cards for free. Small acts. Big ripples. We are the change. Not the system.
Shruti Badhwar
January 10, 2026 AT 19:17
While the clinical recommendations are sound, the implementation of universal screening remains logistically and economically challenging in low-resource settings. The cost-benefit analysis of population-wide G6PD testing must be weighed against the burden of hemolytic crises, hospitalizations, and long-term sequelae. Evidence suggests that targeted screening in high-prevalence regions, coupled with provider education, yields the highest return on investment. Policy change requires data-and we have it.