Understanding Parkinson's Disease and Dementia
As we all know, Parkinson's Disease and Dementia are two separate neurological disorders that affect millions of people worldwide. However, did you know that there is a strong connection between these two conditions? In this article, we will delve into the link between Parkinson's Disease and Dementia, shedding light on how these disorders overlap and how they can impact the lives of those affected. We'll cover the following topics:
1. The Basics of Parkinson's Disease and Dementia
First, let's take a look at the basics of both Parkinson's Disease and Dementia. Parkinson's Disease is a progressive neurological disorder that affects movement, causing tremors, stiffness, and difficulty with balance and coordination. It is caused by the loss of dopamine-producing cells in the brain, which are essential for controlling movement.
Dementia, on the other hand, is a term used to describe a group of symptoms affecting cognitive function, such as memory, thinking, and reasoning. The most common cause of dementia is Alzheimer's disease, but there are several other forms, including vascular dementia, Lewy body dementia, and frontotemporal dementia. These conditions can lead to a decline in a person's ability to perform everyday activities and maintain independence.
2. The Connection Between Parkinson's Disease and Cognitive Decline
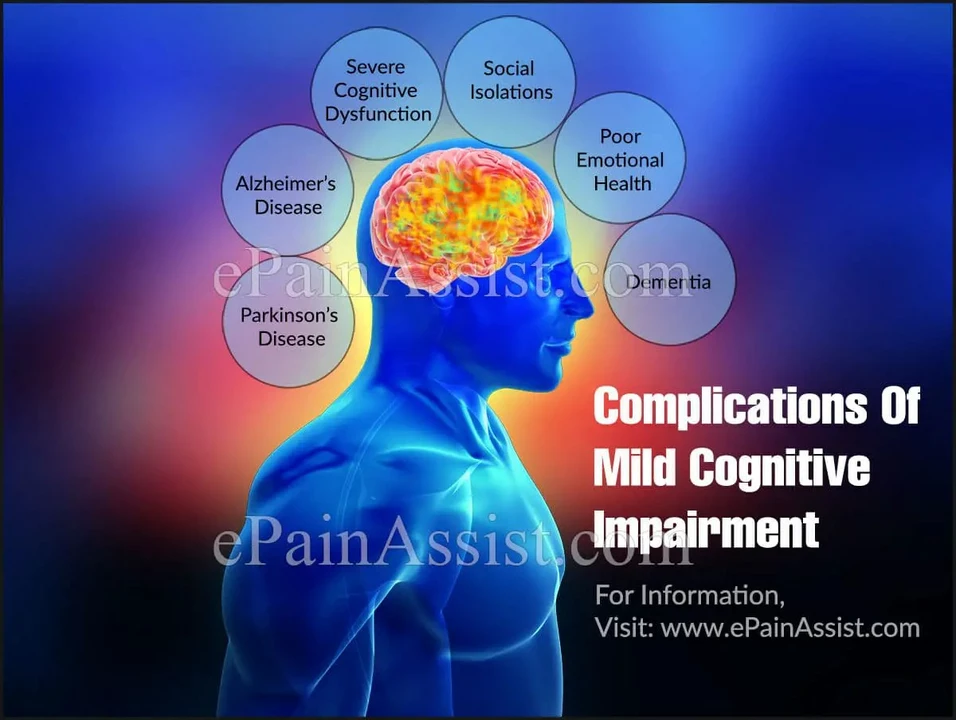
Now that we have a basic understanding of the two conditions, let's discuss the connection between Parkinson's Disease and cognitive decline. Although Parkinson's is primarily known for its impact on movement, it can also cause cognitive changes in some individuals. These cognitive changes can range from mild cognitive impairment to more severe forms of dementia, such as Parkinson's Disease Dementia (PDD).
Research suggests that up to 50% of people with Parkinson's may develop PDD over time. This connection is thought to be due to the same underlying brain changes responsible for the motor symptoms of Parkinson's, such as the loss of dopamine-producing cells and the presence of abnormal protein deposits called Lewy bodies.
3. Symptoms and Diagnosis of Parkinson's Disease Dementia
When it comes to diagnosing Parkinson's Disease Dementia, doctors typically look for a combination of motor symptoms associated with Parkinson's and cognitive symptoms indicative of dementia. Common cognitive symptoms of PDD can include memory problems, difficulty concentrating, and difficulty with problem-solving and decision-making.
It's important to note that a diagnosis of PDD can only be made if cognitive symptoms develop at least one year after the onset of motor symptoms. This is because there is another form of dementia, known as Dementia with Lewy Bodies (DLB), which shares many similarities with PDD, but has a different diagnostic criteria and treatment approach.
4. Treatment and Management of Parkinson's Disease Dementia
Unfortunately, there is no cure for Parkinson's Disease Dementia, but there are treatments and strategies available to help manage the cognitive symptoms and maintain the quality of life for those affected. Some medications used for Alzheimer's disease, such as cholinesterase inhibitors, can help improve cognitive function in some individuals with PDD. Other strategies may include cognitive rehabilitation, occupational therapy, and speech therapy to help with communication and daily living skills.
It's also essential for individuals with PDD and their caregivers to develop a strong support system, including healthcare professionals, family, friends, and support groups. This can help ensure that the person affected by PDD receives the appropriate care and assistance they need as the disease progresses.
5. The Importance of Early Detection and Intervention
Last but not least, early detection and intervention are crucial when it comes to managing both Parkinson's Disease and Dementia. Recognizing the early signs of cognitive decline in someone with Parkinson's can lead to more effective treatment and management strategies, ultimately improving their quality of life and slowing the progression of cognitive decline.
If you or a loved one is experiencing symptoms of Parkinson's Disease or cognitive decline, it's essential to speak with a healthcare professional as soon as possible. With the right care and support, individuals with Parkinson's Disease and Dementia can continue to live fulfilling lives despite the challenges these conditions present.
Brady Johnson
April 30, 2023 AT 05:48
Alright, so the article tries to tie Parkinson's to dementia like it's some grand conspiracy. It’s not a conspiracy, it’s just biology, and the writer glosses over the messy reality. Sure, Lewy bodies show up in both, but they’re not the whole story. The piece also pretends the treatment options are more hopeful than they actually are. Bottom line: don’t take this as a miracle cure guide.
Jay Campbell
May 6, 2023 AT 00:41
I think the article does a decent job laying out the basics without getting too technical, which is helpful for folks new to the topic.
Laura Hibbard
May 11, 2023 AT 19:34
First off, kudos for pulling together a topic that’s often split between neurologists and geriatricians – it’s refreshing to see a holistic view.
That said, let’s unpack what’s really going on here because the devil’s in the details.
The dopaminergic loss that drives the motor symptoms of Parkinson’s also messes with the brain’s executive networks, which explains why some patients develop mild cognitive impairment before full‑blown dementia.
Speaking of Lewy bodies, they’re not just random protein clumps; they’re the same alpha‑synuclein aggregates that underlie both Parkinson’s disease dementia (PDD) and dementia with Lewy bodies (DLB), blurring diagnostic lines.
What the article missed is the role of cholinergic deficits – the same pathway targeted by some Alzheimer’s meds, which is why cholinesterase inhibitors sometimes give modest benefits in PDD.
And let’s not ignore the vascular contributions – hypertension, diabetes, and even sleep apnea can accelerate cognitive decline in Parkinson’s patients, a factor rarely highlighted in lay‑person pieces.
From a research standpoint, recent neuroimaging studies show reduced cortical thickness in the posterior cingulate and precuneus in PDD, mirroring patterns seen in Alzheimer’s disease.
That tells us overlapping pathologies, not just a one‑way street.
Clinically, the one‑year rule separating PDD from DLB is a useful heuristic, but it’s a bit of a fudge factor; patients can swing back and forth on that timeline depending on disease progression.
Early detection, as the article notes, is crucial, but we should stress that regular neuropsychological testing is the gold standard, not just watching for overt memory loss.
The article mentions occupational therapy, which is great, yet it glosses over the importance of tailored cognitive rehabilitation programs that target attention and working memory specifically for Parkinsonian patients.
And let’s be real: caregiving burden is massive – spouses often report burnout within two years of noticeable cognitive decline, so support groups aren’t just nice extras, they’re essential for mental health.
On a hopeful note, there’s emerging evidence that combination therapy – dopaminergic agents plus cognitive enhancers – can slow the trajectory of dementia in Parkinson’s, though large‑scale trials are still pending.
Bottom line: the connection is real, multifactorial, and demands a multidisciplinary approach that mixes neurology, psychiatry, and primary care.
So, while the article gives a solid overview, readers should dig deeper into the nuances if they or a loved one are navigating this complex landscape.
Rachel Zack
May 17, 2023 AT 14:28
Honestly, i cant stand when ppl act like this is just another "age thing" when in fact it’s a serious moral failure to ignore the suffering of those with brain disease. This kind of neglect is unacceptable and we need better policies now.
Lori Brown
May 23, 2023 AT 09:21
Staying positive helps! 😊
Jacqui Bryant
May 29, 2023 AT 04:14
I really think the article gave some good tips, but it could have said more about how simple daily exercises can keep the brain active. Even short walks or light stretching can make a difference, and that's something anyone can do.
Paul Luxford
June 3, 2023 AT 23:08
It's important to remember that each patient's journey is unique, so personalized care plans are essential. Respecting boundaries while offering resources makes a big difference.
Nic Floyd
June 9, 2023 AT 18:01
🧠 When you talk about PDD, you gotta consider the interplay of α‑synucleinopathies and cholinergic deficits – it’s a neurochemical cocktail that’s not trivial. Also, from a pharmaco‑economic perspective, cost‑effectiveness analyses of cholinesterase inhibitors in PDD are still emerging, so clinicians should stay updated on the latest health‑policy guidelines. In short: integrate the neuropharmacology with real‑world data, and you'll get a clearer picture of therapeutic windows. 🌐