Excretion: How Your Body Removes Drugs and Waste
Excretion is how your body gets rid of stuff it doesn’t need — from worn-out cells to drugs you took yesterday. Think of it as the clean-up crew: kidneys, liver, lungs, skin and gut all pitch in. Knowing how excretion works helps you understand side effects, drug timing, and why your doctor checks kidney or liver tests before changing a dose.
Most drugs leave the body through urine or bile. Kidneys filter blood and push water-soluble compounds into urine. The liver often changes drugs into forms that dissolve in water, then sends them to bile or blood for kidney clearance. Lungs excrete gases like anesthetics, skin loses tiny amounts in sweat, and the gut can expel drug residues in feces. Which route matters — it changes how fast a drug stops working and who needs dose changes.
Practical signs and tests
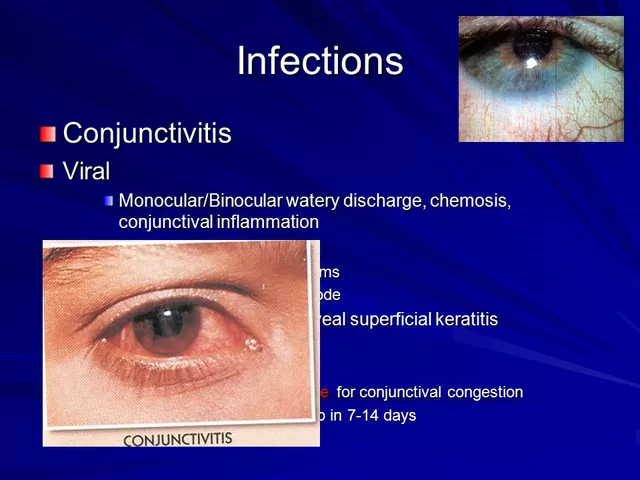
You can spot excretion issues early. Dark urine, persistent swelling, less peeing, or extreme tiredness can hint at poor kidney excretion. Yellowing skin or belly pain may point to liver problems. Simple lab tests — creatinine, estimated glomerular filtration rate (eGFR) for kidneys, and ALT/AST for liver — tell the real story. If you take medicines cleared by kidneys or liver, keep recent test results handy for prescribers.
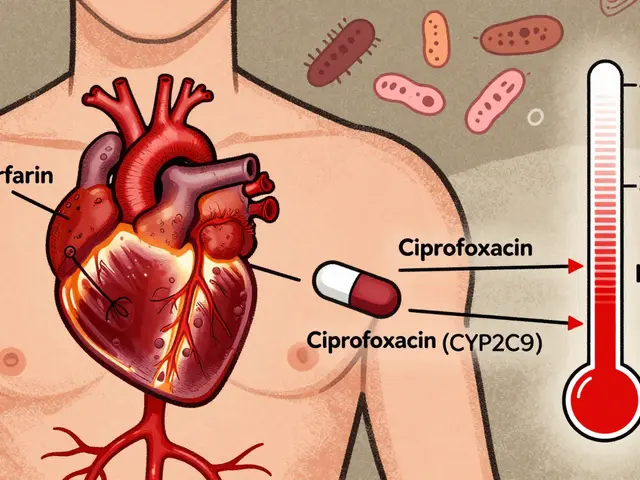
How excretion affects your medicines
If your kidneys slow down, drugs that leave through urine build up and cause stronger effects or toxicity. That’s why doctors lower doses or increase the time between doses for some antibiotics, blood pressure meds, and diabetes drugs. Liver disease changes how drugs are broken down; some medications stay active longer. Even things like hydration, salt intake, and other drugs can speed up or slow down excretion — antacids, grapefruit juice, diuretics, and certain supplements all interact.
Want actionable steps? First, tell your doctor about every medicine and supplement you take. Second, stay hydrated but avoid huge fluid swings right before tests. Third, bring a list of medicines when you get lab results; pharmacists can flag dosage problems. Fourth, report changes: less urine, new yellowing, or sudden dizziness deserve a call to your clinician.
Special groups need extra care. Older adults naturally have slower kidney function, so doses that worked when you were 40 might be too high at 70. Babies and pregnant people process drugs differently, too. Hospitals adjust doses for all these groups and monitor levels when necessary — for example with certain heart or seizure drugs where small changes become risky.
Understanding excretion helps you avoid surprises. If a medication folder warns “dose adjust in renal impairment,” don’t ignore it. Ask how and when blood tests will check your organs, and if side effects could come from slowed excretion. With the right monitoring and simple lifestyle steps, you and your prescriber can keep medicines safe and effective.
Examples: older patients often need smaller doses of antibiotics like gentamicin and some diabetes drugs need longer gaps between doses. Ask your pharmacist how kidney or liver tests change your schedule — they can suggest safer timing or dose changes today.