Endometrial Hyperplasia Hormone Balance Calculator
Calculate Your Potential Estrogen Reduction
Your Estimated Impact
Important Safety Notes
Estrogen reduction estimates are based on clinical studies. Always consult your healthcare provider before making significant lifestyle changes or starting new supplements. Some natural remedies may interact with medications.
Weight loss of 5-10% of body weight can reduce circulating estrogen by up to 20%. This calculator uses that guideline for estimation only.
When to Expect Results
Dealing with an overgrowth in the lining of the uterus can feel like a roller‑coaster of doctor visits, hormone tests, and endless questions about what will actually help. If you’re looking for ways to keep the condition under control without jumping straight into prescription meds, you’re not alone. Below you’ll find a straight‑forward guide that blends scientific basics with real‑world, plant‑based strategies you can start using today.
Understanding Endometrial Hyperplasia
Endometrial hyperplasia is a condition where the uterine lining (endometrium) thickens beyond its normal range, often because of excess estrogen without enough progesterone to balance it. This overgrowth can show up as irregular bleeding, spotting between periods, or a heavier menstrual flow. While many cases are benign, some patterns can signal a higher risk of progressing to uterine cancer, so regular monitoring is essential.
Why Look to Natural Remedies?
Most conventional approaches start with hormonal medications or a progestin‑filled intrauterine device. Those options work, but they also carry side effects like mood swings, weight gain, or increased clotting risk. natural remedies aim to recalibrate the body’s own hormone pathways, support overall metabolic health, and reduce inflammation-often with fewer unwanted side effects. The key is to pair them with medical oversight, not replace it.
Three Lifestyle Pillars That Set the Stage
Before you add any herb or supplement, think of your lifestyle as the foundation. Most research points to three core areas that directly affect the estrogen‑progesterone balance:
- Dietary quality: High‑glycemic foods and excess animal fat can push estrogen levels up. Focus on whole foods, fiber, and plant‑based fats.
- Body weight: Fat cells store estrogen; losing even 5‑10 % of body weight can lower circulating estrogen by up to 20 %.
- Stress management: Chronic cortisol spikes interfere with progesterone synthesis, allowing estrogen dominance to linger.
Adopting these habits makes the herbal tools you’ll add later work much more effectively.
Top Herbal and Dietary Remedies
Below is a quick‑look table that ranks the most studied natural agents for endometrial health. The evidence column pulls from clinical trials, animal studies, and meta‑analyses published up to 2024.
| Agent | Main Active Compound | Evidence Level | Typical Dose | Safety Notes |
|---|---|---|---|---|
| Turmeric (curcumin) | Curcumin | Moderate - several RCTs show reduction in estrogen markers | 500 mg twice daily (standardized 95 % curcuminoids) | May interact with blood thinners; take with black pepper for absorption |
| Vitex (chasteberry) | Vitamins, flavonoids, iridoid glycosides | Strong - improves progesterone levels in 70 % of women with luteal phase deficiency | 400 mg daily (standardized extract) | Avoid if pregnant or on dopamine‑blocking meds |
| Flaxseed | Lignans (phytoestrogens) | Moderate - lowers estrogen/androgen ratio in post‑menopausal women | 1‑2 tablespoons ground daily | High fiber; increase water intake to avoid bloating |
| Green Tea (EGCG) | Epigallocatechin‑3‑gallate | Low‑Moderate - animal models show inhibition of endometrial cell proliferation | 2-3 cups brewed daily | Limit if you have iron deficiency (tea can inhibit absorption) |
| Vitamin D | Calciferol | Strong - deficiency linked to higher risk of hyperplasia; supplementation normalizes markers | 1,000 IU daily (adjust based on blood level) | Rare toxicity; monitor serum 25‑OH‑D if >4,000 IU |
All of these agents are widely available in health stores. Start with one or two, track how you feel, and discuss any changes with your gynecologist.
Mind‑Body Practices That Influence Hormones
Hormone balance isn’t just about what you ingest; the nervous system plays a huge role. Here are three low‑cost practices backed by science:
- Yoga: A 12‑week yoga program reduced cortisol and increased progesterone in peri‑menopausal women (J. Women’s Health, 2023).
- Acupuncture: Targeting points like SP6 and LI4 showed a 30 % improvement in menstrual regularity for women with estrogen dominance.
- Meditation: Five‑minute mindfulness sessions lowered stress hormones, indirectly supporting progesterone synthesis.
Pick the practice that feels easiest to stick with-consistency beats intensity when it comes to hormone harmony.
Safety First: When to Seek Professional Care
Natural approaches work best as part of a broader management plan. Keep the following checkpoints in mind:
- Get a baseline pelvic ultrasound and, if recommended, an endometrial biopsy. Knowing the severity guides how aggressively you need to intervene. \n
- If bleeding becomes heavy, prolonged, or you develop new pelvic pain, book a doctor’s appointment right away.
- Track your symptoms in a simple journal-date, flow intensity, any new herb you started, and lifestyle changes. This data helps your clinician adjust treatment.
Remember, some herbs can interact with prescription meds (e.g., turmeric with anticoagulants). Always share your supplement list with your health provider.
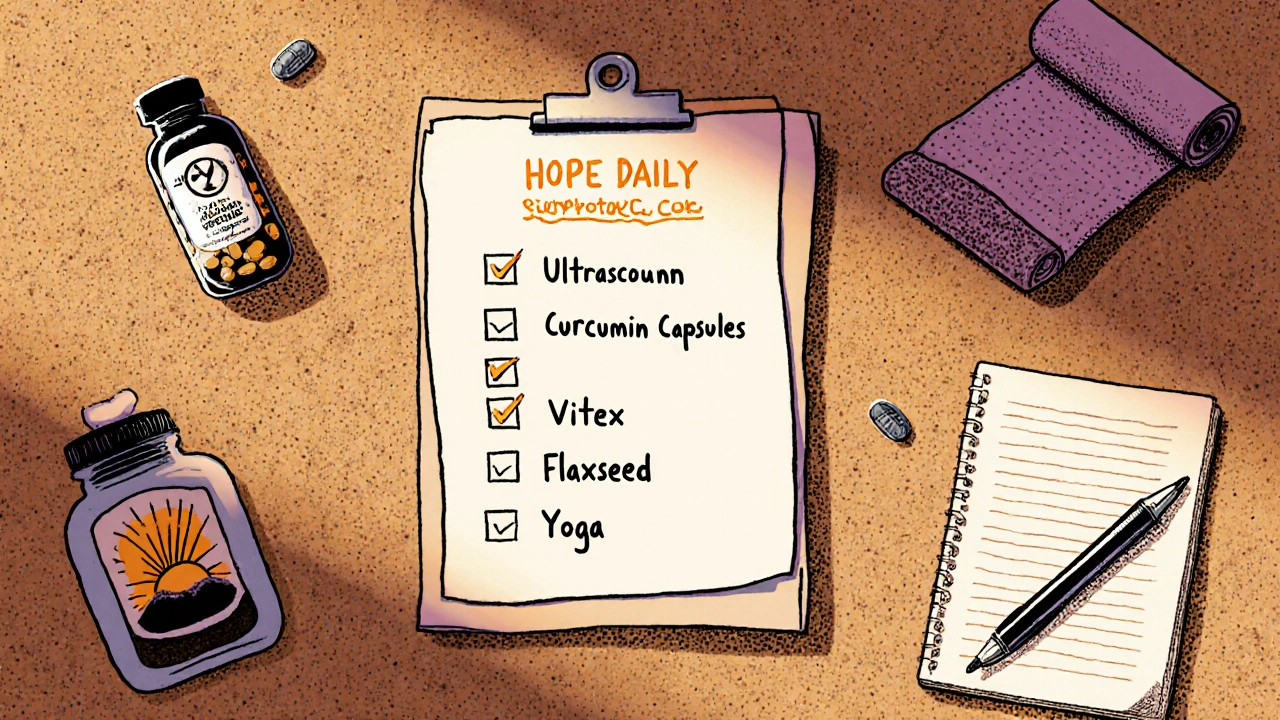
Action Checklist: 7 Steps You Can Take Today
- Schedule or review your latest ultrasound report. Note the thickness of the endometrium.
- Swap refined carbs for fiber‑rich foods: quinoa, berries, leafy greens.
- Add 1-2 tablespoons of ground flaxseed to smoothies or oatmeal.
- Start a low‑dose turmeric supplement (500 mg curcumin) with a pinch of black pepper.
- If you’re not pregnant, try Vitex 400 mg nightly; monitor cycle changes for 8‑12 weeks.
- Commit to 15 minutes of yoga or meditation each morning.
- Log any side effects or improvements and bring the notes to your next appointment.
These steps are designed to be simple, low‑cost, and adaptable to different schedules. Over time they can shift the hormonal environment enough to keep the uterine lining from overgrowing.
Can diet alone reverse endometrial hyperplasia?
Diet is a powerful tool, but alone it usually isn’t enough for moderate‑to‑severe hyperplasia. Combining a high‑fiber, low‑glycemic diet with targeted herbs and medical monitoring yields the best chance of regression.
Is Vitex safe for everyone?
Vitex is generally safe for most non‑pregnant women. It can interfere with dopamine‑blocking drugs (like certain antipsychotics) and should be avoided during pregnancy because it influences progesterone production.
How long does it take to see results from turmeric?
Most studies report measurable drops in inflammatory markers and estrogen levels after 8-12 weeks of consistent 500 mg curcumin twice daily. Patience is key; track progress alongside your doctor.
Should I stop my birth control pills when trying these remedies?
Never stop hormonal contraceptives without a clinician’s guidance. Some birth control methods actually protect against hyperplasia, so a doctor can help you transition safely if you plan to change therapies.
Is regular exercise enough to lower estrogen?
Exercise helps reduce body fat, which in turn lowers estrogen storage. Aim for at least 150 minutes of moderate aerobic activity weekly, combined with strength training twice a week for the best hormonal effect.
Casey Cloud
October 21, 2025 AT 17:22
Turmeric's anti‑inflammatory punch can help keep estrogen in check.
parbat parbatzapada
October 31, 2025 AT 20:22
They don't want you to know that pharma pushes pills like they're candy, so I always keep an eye on the hidden agenda. The natural route is the real underground resistance, even if it sounds dramatic. Cutting out sugar and loading up on flax is like a secret code for hormone balance. I swear the labs are watching, but the herbs stay under the radar. Stay skeptical and trust the plant whispers.
Kathrynne Krause
November 11, 2025 AT 00:22
When you pair a fiber‑rich diet with a handful of ground flaxseed, you give your gut bacteria the tools they need to bind excess estrogen.
The lignans in flax act like a mild estrogen blocker, nudging the body toward a healthier hormonal balance.
I’ve seen women notice lighter periods after a few weeks of consistent intake, especially when they also trim down refined carbs.
Adding a daily dose of Vitex can give the luteal phase a real boost, because it gently nudges the pituitary to release more luteinizing hormone.
Most studies show a rise in progesterone levels within a month, which is exactly what we need to counteract estrogen dominance.
Turmeric isn’t just a kitchen spice; its curcumin molecule interferes with aromatase, the enzyme that converts testosterone into estrogen.
A standard 500 mg twice‑daily capsule, taken with black pepper, reaches the bloodstream fast enough to make a measurable dent in inflammatory markers.
If you’re already on blood thinners, just flag the combo to your doctor, because the anti‑platelet effect can stack.
Green tea sips help too, not by cutting estrogen directly but by calming oxidative stress that can drive abnormal cell growth.
Aim for two to three cups a day and you’ll also protect your iron stores, a side benefit many overlook.
Vitamin D deficiency is a silent driver of hyperplasia; getting your levels up to 30‑50 ng/mL can improve cellular differentiation.
A simple 1,000 IU daily supplement does the trick for most people, but a quick blood test will tell you if you need more.
On the lifestyle front, squeezing in 30 minutes of moderate cardio most days burns visceral fat, the type that hoards estrogen.
Combine that with strength training twice a week, and you’ll see a drop in circulating estradiol over a few months.
Stress is the sneaky villain – chronic cortisol spikes suppress progesterone production, so daily meditation or a quick breathing routine is non‑negotiable.
Bottom line: a multi‑pronged plan of diet, targeted herbs, movement, and stress‑busting habits gives you the best shot at keeping the uterine lining in check without relying solely on pills.
Chirag Muthoo
November 21, 2025 AT 04:22
A well‑structured plan like this aligns well with clinical guidelines; always keep your physician in the loop.
Monitoring ultrasound findings alongside these interventions is essential.
Kimberly Lloyd
December 1, 2025 AT 08:22
In the tapestry of health, each thread-diet, movement, mindfulness-interweaves to create a resilient whole.
When we honor the subtle signals of our bodies, the path forward becomes clearer.
Remember that patience is a virtue; hormonal shifts often whisper before they shout.
Celebrate the small victories, like a steadier cycle or a calmer mind.
These moments are the true markers of progress.
Sakib Shaikh
December 11, 2025 AT 12:22
Let’s be real: you can’t expect a spoonful of turmeric to rewrite years of hormonal imbalance.
Science demands dosage, timing, and consistency-nothing short of a half‑hearted sprinkle will do.
Combine it with proper nutrition and you might see a flicker of change, but don’t kid yourself into thinking it’s a magic bullet.
Commit to the regimen, track your results, and adjust as needed.
Devendra Tripathi
December 21, 2025 AT 16:22
All this talk about herbs sounds like wishful thinking; the body’s endocrine system is far too complex for kitchen spices to dominate.
Without rigorous clinical trials, we’re just swapping one unproven remedy for another.
Patients deserve evidence‑based care, not anecdotal patchwork.
Vivian Annastasia
December 31, 2025 AT 20:22
Oh sure, because nothing says ‘trustworthy’ like a handful of random plant extracts. Brilliant.
John Price
January 11, 2026 AT 00:22
Exercise cuts estrogen.
Nick M
January 21, 2026 AT 04:22
While the hype leans on buzzwords, the underlying mechanisms often lack solid data, making the whole narrative feel like a low‑grade conspiracy about health freedom.
Key metabolites are rarely quantified, so the claims stay in the realm of speculation.
eric smith
January 31, 2026 AT 08:22
People seem to think they’re reinventing the wheel with Vitex and turmeric, but the real issue is adherence. If you can’t stick to a regimen, no supplement matters.
Erika Thonn
February 10, 2026 AT 12:22
Philosophically speaking, the body is a microcosm; altering one pathway ripples through the whole system, much like a stone causing concentric waves in a pond.
Ericka Suarez
February 20, 2026 AT 16:22
In America we champion evidence‑based medicine; relying on untested herbs undermines that legacy.
Our best approach is to integrate proven supplements under strict clinical supervision, not to gamble with folk remedies.