Blood Pressure Medication Comparison: Guides, Prices, and What Works Best
When working with blood pressure medication comparison, the process of evaluating different antihypertensive drugs side‑by‑side to find the right fit for a patient. Also known as BP drug comparison, it helps clinicians and patients weigh effectiveness, side effects, cost, and monitoring needs. This effort often involves antihypertensive drugs, medicines that lower arterial pressure such as ACE inhibitors, beta‑blockers, calcium‑channel blockers, and diuretics and sometimes overlaps with direct oral anticoagulants, blood‑thinning agents like apixaban or rivaroxaban that can affect overall cardiovascular risk. Understanding these connections is essential because a change in one class can shift the need for another, especially in patients with heart failure or atrial fibrillation.
Key drug classes to compare
First up are ACE inhibitors, drugs that block the conversion of angiotensin I to angiotensin II, resulting in vasodilation and lower blood pressure. They are prized for kidney protection but may cause a dry cough. Next, beta‑blockers, agents that reduce heart rate and contractility, often used after a heart attack. Their downside can be fatigue or slowed metabolism. Calcium‑channel blockers, like amlodipine, relax arterial smooth muscle, offering a good option for isolated systolic hypertension, while diuretics, especially thiazides, remove excess fluid and sodium to bring pressure down. Each class has a distinct efficacy profile, typical dosing range, and monitoring requirement, so a thorough comparison looks at all three attributes—effectiveness, safety, and cost.
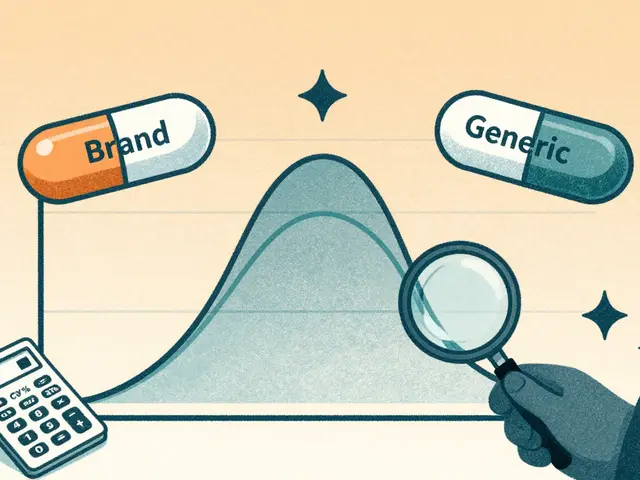
To run a solid comparison you start with three data points: clinical efficacy (how much the drug lowers systolic/diastolic pressure), safety profile (common and serious side effects), and total cost of therapy (price per month, insurance coverage, generic availability). Tools like online price calculators, pharmacist consultations, and treatment guidelines let you rank each drug on these dimensions. You also need to consider patient‑specific factors such as age, kidney function, and comorbidities like diabetes or atrial fibrillation. By scoring each medication against these criteria, you create a personalized ranking that goes beyond generic “best drug” lists and reflects real‑world needs.
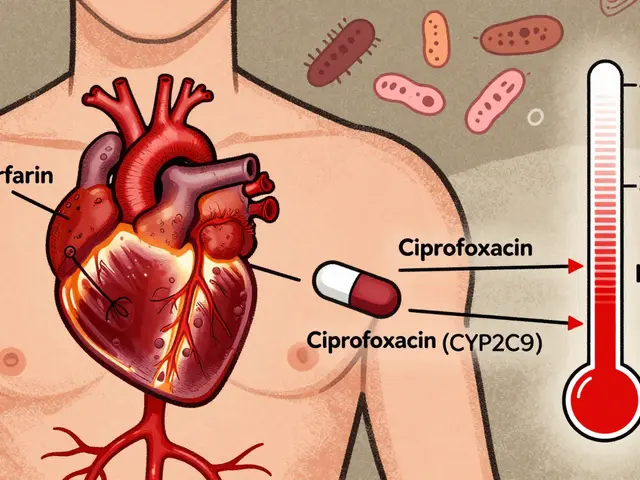
When you add anticoagulants into the mix, the picture gets more nuanced. For example, warfarin, a traditional vitamin K antagonist, needs regular INR checks and interacts with many foods and drugs, while newer direct oral anticoagulants such as apixaban or rivaroxaban have fixed dosing and fewer dietary restrictions but come at a higher price. A blood pressure medication comparison therefore has to factor in whether a patient is on a blood thinner, because bleeding risk can influence the choice of antihypertensive—some agents like ACE inhibitors may raise potassium levels, which could be problematic with certain anticoagulants. The posts below walk you through price checks, safety tips, and side‑by‑side tables for popular choices, from generic well‑known brands to the latest oral anticoagulants. Whether you’re a clinician building a formulary, a patient reviewing options, or a shopper hunting the best deal, the upcoming guides give you the facts you need to make an informed decision without guesswork.