Diuretics: How They Work, Types, and Safety Tips
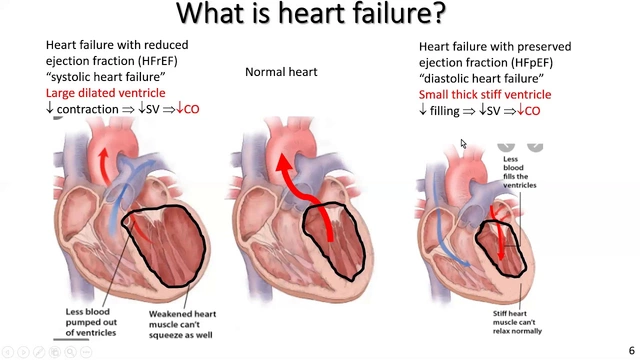
Diuretics—often called "water pills"—help your body remove extra salt and water. Doctors prescribe them for high blood pressure, fluid buildup from heart failure, kidney problems and some forms of swelling. They’re simple drugs but can change how your body handles salt, potassium and fluid, so a little know‑how makes them safer and more effective.
Common types and what they do
There are three types you’ll hear about most:
Loop diuretics (like furosemide/Lasix) are strong. They remove a lot of fluid fast and are used for heart failure or major swelling.
Thiazide diuretics (hydrochlorothiazide, chlorthalidone) are a first choice for high blood pressure. They work slower and lower blood pressure reliably at low doses.
Potassium‑sparing diuretics (spironolactone, amiloride) are weaker but help keep potassium from dropping too low. Doctors often combine them with other diuretics.
Use them safely — practical tips
Timing matters: take daytime doses to avoid waking at night to urinate. If you need more than one dose a day, take the last dose in the mid‑afternoon.
Watch your weight. A quick gain of 2–3 pounds in 24 hours can signal fluid retention. Track daily weight if you have heart failure and tell your doctor about sudden changes.
Electrolytes are key. Diuretics can lower potassium, sodium, magnesium and change kidney function. Your doctor will want blood tests after starting or changing doses. If you feel weak, dizzy or have muscle cramps, check your potassium.
Avoid mixing with some drugs. NSAIDs (ibuprofen, naproxen) can blunt diuretic effects. Combining diuretics with ACE inhibitors or ARBs needs monitoring because blood pressure and kidney function can drop. Tell your prescriber about all medicines and supplements.
Stay hydrated but don’t overdo it. If you’re sweating a lot or have vomiting or diarrhea, you may need medical advice about fluids and electrolytes rather than stopping diuretics yourself.
Salt matters. Cutting back on table salt helps diuretics work better. But for some people—especially those on potassium‑sparing drugs—potassium supplements or high‑potassium diets can be risky unless your doctor approves.
Travel and surgery: bring a medication list and ask whether you should stop a diuretic before procedures. Hospitals sometimes hold diuretics around surgery because of fluid shifts and monitoring needs.
Know when to call: fainting, extreme weakness, irregular heartbeat, very low urine output, severe dizziness, or signs of dehydration need urgent attention.
Want more detail on a specific drug? Our Lasix (furosemide) article covers how that loop diuretic works, common side effects and practical tips for use. Read detailed guides or ask your clinician for a plan that matches your condition and daily life.
Diuretics are powerful tools when used right. With simple checks—weight, bloods and clear communication with your doctor—you can get benefits while keeping risks low.