TZD Fluid Retention Calculator
This calculator estimates your expected fluid and fat weight gain from TZD medications based on clinical data. Most weight gain from TZDs is fluid (65-70%), not fat. Monitoring is crucial because sudden weight gain (>2-3 kg in a week) indicates serious fluid retention.
Results
Expected Total Weight Gain
This is an estimate based on clinical studies
Fluid Retention Breakdown
When you're managing type 2 diabetes, getting your blood sugar under control is the goal. But for some people, taking a TZD like pioglitazone or rosiglitazone brings an unexpected problem: sudden weight gain and swollen ankles. It’s not just about gaining a few pounds-it’s about fluid building up in your body, making shoes too tight, legs feel heavy, and breathing harder after climbing stairs. This isn’t rare. About 1 in 3 people on TZDs experience noticeable edema, and nearly 6 out of 10 gain weight. The good news? You don’t have to just live with it. There are real, proven ways to cut these side effects down-without giving up the benefits of better insulin sensitivity.
Why TZDs Cause Weight Gain and Swelling
TZDs work by making your body’s cells more responsive to insulin. That’s great for lowering blood sugar, especially if you have severe insulin resistance. But here’s the catch: the same mechanism that helps your muscles use glucose also tricks your kidneys into holding onto sodium and water. This isn’t fat gain-it’s fluid. Studies show that 65-70% of the weight gain from TZDs comes from extra fluid, not fat. Your body’s fluid volume increases, and that extra water collects in your lower legs, feet, and sometimes even your abdomen.
The science behind it is complex, but it boils down to a few key actions in your kidneys. TZDs turn on sodium transporters in the tubules-especially the ones that reabsorb sodium instead of letting it leave in your urine. This causes your blood volume to rise, which increases pressure in your capillaries. Fluid then leaks into surrounding tissues, causing swelling. At the same time, TZDs trigger the release of vascular endothelial growth factor, which makes blood vessel walls more permeable, letting even more fluid escape into your tissues.
It’s worse if you’re already on insulin. Combining TZDs with insulin can push edema rates up to 16%. That’s why doctors are extra cautious when prescribing both together. And if you’ve got heart problems, especially moderate to severe heart failure (NYHA Class III or IV), TZDs are off-limits. The extra fluid can overwhelm your heart, making symptoms worse.
How Much Weight and Swelling Are You Really Gaining?
Numbers matter here. On average, people on pioglitazone gain about 3 kg (6.6 lbs) in the first few months. Rosiglitazone adds about the same. But the real red flag isn’t the scale-it’s how fast the weight comes on. Gaining more than 2-3 kg (4-6.5 lbs) in a week is a warning sign. That’s not normal fat gain. That’s fluid retention building up fast.
Swelling usually shows up in your ankles and feet first. You might notice your rings don’t fit, your shoes feel tighter, or your socks leave deep marks. Some people report their legs feeling “heavy” or “wooden.” In more serious cases, swelling can spread to the lower back or even cause shortness of breath if fluid builds up around the lungs.
One study tracking 1,245 TZD users found that 63% noticed visible edema. And in online diabetes communities, 82% of people who stopped their TZD did so because of swelling or weight gain. That’s not just inconvenience-it’s quality of life.
Three Proven Ways to Reduce Fluid Retention
You don’t have to choose between good blood sugar control and feeling bloated. Here are three strategies backed by clinical data that actually work.
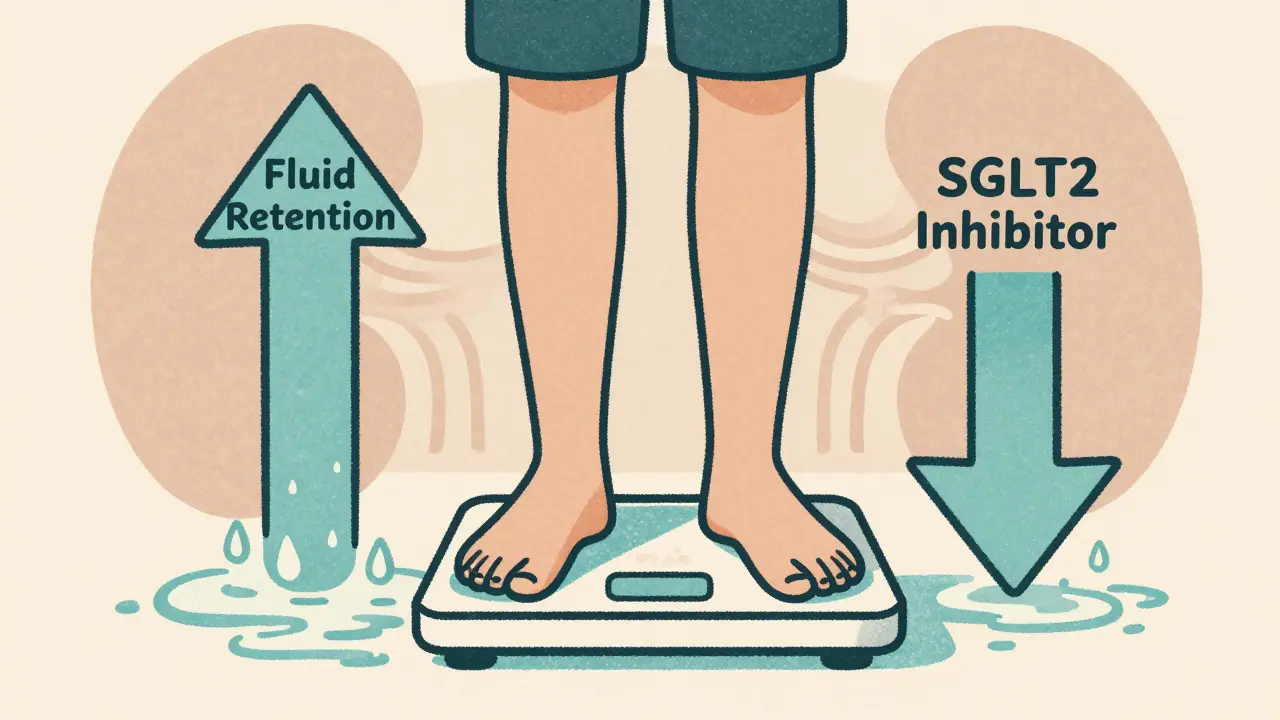
1. Combine TZDs with SGLT2 Inhibitors
This is the most effective strategy. SGLT2 inhibitors like empagliflozin, dapagliflozin, or canagliflozin make your kidneys dump sugar-and water-out through urine. They counteract the fluid-retaining effects of TZDs. In a 2020 study, adding an SGLT2 inhibitor to pioglitazone cut edema rates by 45%. That’s huge. You still get the insulin-sensitizing power of the TZD, but the SGLT2 inhibitor pulls the excess fluid out before it builds up.
Plus, SGLT2 inhibitors often cause modest weight loss, improve blood pressure, and protect your heart. They’re now first-line options for many people with type 2 diabetes, especially those with heart or kidney risks. If you’re on a TZD and still struggling with swelling, talk to your doctor about switching or adding one of these.
2. Lower the Dose-Slowly
You don’t need the highest dose to get results. Pioglitazone at 15 mg daily causes only 2.1% edema, while 45 mg pushes it to 4.8%. That’s more than double the risk for the same benefit. Most guidelines now recommend starting at 15 mg and only increasing if needed after 3-4 months. Many patients do just fine on the lowest dose.
Same goes for rosiglitazone. The 4 mg dose has a 4.8% edema rate. Going higher doesn’t improve blood sugar much but increases side effects. Less is often more.
3. Use a Diuretic-But Choose Wisely
If fluid retention is stubborn, your doctor might suggest a mild diuretic. But not all diuretics are equal. Loop diuretics like furosemide are strong and can cause electrolyte imbalances, especially in older adults or those with kidney issues. Thiazide diuretics like hydrochlorothiazide are gentler and better suited for TZD-related swelling. They help flush out sodium without overworking your kidneys.
One observational study found thiazides reduced edema by 38% in TZD users. They’re not a cure-all, but when used carefully, they can make a real difference.

Lifestyle Tweaks That Actually Help
Medications aren’t the only tools. Simple daily habits can reduce swelling significantly.
- Limit sodium to under 2,000 mg per day. That means avoiding processed foods, canned soups, deli meats, and restaurant meals. Read labels. Even small reductions in salt intake can cut fluid retention by 27%, according to one clinical trial.
- Elevate your legs. When you’re sitting or lying down, prop your feet up on a pillow. This helps gravity pull fluid back toward your heart instead of letting it pool in your ankles.
- Move regularly. Walking for 20-30 minutes a day keeps your circulation going and helps prevent fluid from settling. Avoid sitting for long periods.
- Check your weight daily. Weigh yourself at the same time each morning, after using the bathroom and before eating. A jump of 2 lbs or more in 24 hours is a red flag. Report it to your doctor right away.
One study showed that patients who tracked their weight daily had 34% fewer hospitalizations for heart failure. It’s a small habit with a big impact.
When to Stop TZDs Altogether
Not everyone can tolerate them. If you’ve tried lowering the dose, adding an SGLT2 inhibitor, cutting salt, and still have:
- Swelling that doesn’t improve
- Shortness of breath at rest
- Weight gain over 3 kg in a week
- Difficulty lying flat because of breathing issues
Then it’s time to reconsider. TZDs are not worth the risk if they’re pushing you toward heart failure. Your doctor may switch you to a GLP-1 receptor agonist like semaglutide or liraglutide. These drugs improve blood sugar, often cause weight loss, and have proven heart benefits. Or you might go back to metformin, which doesn’t cause weight gain or fluid retention at all.
The bottom line: TZDs are powerful-but they’re not for everyone. They’re best suited for younger, leaner patients with severe insulin resistance who don’t have heart or kidney problems. If you’re older, overweight, or have any signs of heart strain, there are safer, more effective options now.
The Bigger Picture: Why TZDs Are Falling Out of Favor
Back in 2006, TZDs made up nearly 18% of type 2 diabetes prescriptions in the U.S. Today, that number is under 5%. Why? Because safer, more effective drugs came along. SGLT2 inhibitors and GLP-1 agonists don’t just control blood sugar-they protect your heart and kidneys. They help you lose weight. They reduce hospitalizations. And they don’t make your legs swell.
The FDA added a black box warning for heart failure in 2007. Rosiglitazone was pulled from general use in 2010 (though later reinstated with restrictions). Pioglitazone carries a warning about possible bladder cancer risk. These drugs are no longer first- or even second-line. They’re third-line-reserved for cases where other drugs haven’t worked and insulin resistance is extreme.
Even the American Diabetes Association now says TZDs should only be used after careful risk-benefit analysis. Monthly check-ins for the first three months are recommended. And if you’re on one, you need to be monitored closely.
What’s Next? Newer Drugs That Might Replace Them
Researchers are working on next-generation PPAR-γ modulators that keep the insulin-sensitizing benefits but ditch the fluid retention. One drug, saroglitazar, approved in India, cuts edema risk by 60% compared to traditional TZDs. Early trials show promise. If approved in the U.S., it could bring back the benefits of TZDs without the downsides.
There’s also early research into genetic testing. Some people carry a gene variant (rs1801282) that makes them 2.3 times more likely to develop edema on TZDs. In the future, a simple blood test might tell you if this drug is safe for you-or if you should avoid it entirely.
For now, though, the best approach is simple: know your risks, monitor your body, and don’t be afraid to ask for alternatives. You don’t have to accept swelling and weight gain as the price of good blood sugar control.
Can TZDs cause heart failure?
Yes. TZDs can cause or worsen heart failure by increasing fluid volume in the body. That’s why they carry a black box warning from the FDA. They should never be used in people with NYHA Class III or IV heart failure. Even in people without diagnosed heart failure, TZDs can trigger symptoms like shortness of breath, swelling, and fatigue. If you’re on a TZD and notice these symptoms, contact your doctor immediately.
Is weight gain from TZDs fat or fluid?
Most of it is fluid. Studies show 65-70% of the weight gain comes from water retention, not fat. The rest is due to increased fat storage in subcutaneous tissue. But because fluid builds up quickly, sudden weight gain-like 2-3 kg in a week-is almost always fluid. That’s why daily weight checks are so important.
Do all TZDs cause the same side effects?
Rosiglitazone and pioglitazone cause similar levels of fluid retention and weight gain. But pioglitazone has a slightly better safety profile when it comes to heart health. Rosiglitazone was linked to higher heart attack risk in early studies, leading to restrictions. Pioglitazone is now the preferred TZD when one is needed.
Can I take a diuretic with my TZD?
Yes, but only under medical supervision. Thiazide diuretics like hydrochlorothiazide are preferred over loop diuretics because they’re gentler and better for long-term use. They can reduce edema by about 38%. But they can also lower potassium and sodium too much, so blood tests are needed to monitor for imbalances.
Are there alternatives to TZDs for insulin resistance?
Yes. Metformin is the first choice-it improves insulin sensitivity without weight gain. GLP-1 receptor agonists like semaglutide and liraglutide are even better-they reduce insulin resistance, promote weight loss, and protect your heart. SGLT2 inhibitors also improve insulin sensitivity and reduce fluid retention. These are now preferred over TZDs for most patients.
How long does it take for TZD-related swelling to go away after stopping?
Most people see improvement within 1-2 weeks after stopping the drug. Fluid retention starts to reverse as your kidneys begin excreting sodium again. Swelling in the legs and feet usually resolves completely within 3-4 weeks. If swelling persists beyond that, you should be evaluated for other causes like heart, kidney, or liver problems.
What to Do Next
If you’re on a TZD and experiencing swelling or weight gain, don’t ignore it. Start by checking your weight every morning. Track your salt intake. Note any changes in your ankles or breathing. Then talk to your doctor. Ask: Is this dose necessary? Could I switch to an SGLT2 inhibitor? Are there safer alternatives? You have options. You don’t have to accept side effects as part of the deal.
The goal isn’t just to control blood sugar. It’s to live well-without swollen legs, without breathlessness, without the fear that your medicine is making you sicker. The right combination of drugs, lifestyle changes, and monitoring can make all the difference.
Kinnaird Lynsey
December 20, 2025 AT 11:44
I swear, my ankles looked like overinflated balloons after two months on pioglitazone. Didn't even realize it was the med until my shoes started screaming at me. Switched to empagliflozin and within a week, my socks didn't leave trenches. Also lost 4 lbs. Win-win.
Also, why is everyone still prescribing these like they're 2008?
Glen Arreglo
December 20, 2025 AT 18:08
Look, I get it - fluid retention sucks. But if you’re gonna blame the drug, at least know the science. TZDs aren’t magic. They’re fixing insulin resistance, which is the root problem. The swelling? It’s a trade-off. The real issue is doctors not adjusting doses or adding SGLT2s early enough. Stop treating symptoms and start treating the system.
shivam seo
December 22, 2025 AT 17:06
This whole post is Big Pharma whispering into your ear. They want you to swap one pill for another. Meanwhile, the real fix? Cut carbs. Stop drinking soda. Walk more. No drug is gonna fix your lifestyle. But hey, keep taking the pills - I hear the stock price on SGLT2s is doing great.
benchidelle rivera
December 23, 2025 AT 10:50
I cannot believe how casually some people dismiss fluid retention as a "minor side effect." This is not a cosmetic issue. This is cardiovascular strain. If you are gaining more than two kilograms in a week while on a TZD, you are in danger. You are not "just bloated." You are accumulating intravascular volume that your heart cannot manage. This is not a suggestion. This is a medical emergency waiting to happen. Contact your provider immediately. Do not wait.
Andrew Kelly
December 24, 2025 AT 08:14
Funny how they never mention that the FDA black box warning was pushed through after a few cherry-picked studies and a media panic. Rosiglitazone got crucified for a 0.5% increased risk of MI - but nobody talks about how metformin causes lactic acidosis in 0.03% of cases and no one screams about that. And now they’re pushing GLP-1s like they’re holy water. $1000/month injections that make you vomit for six months? Yeah, thanks. I’ll stick with my 15mg pioglitazone and my low-sodium diet. The real conspiracy? They want you addicted to expensive drugs, not cured.
Anna Sedervay
December 25, 2025 AT 21:09
The notion that one can simply "lower the dose" of a thiazolidinedione and expect sustained glycemic control is, frankly, a gross oversimplification of the pharmacodynamics of PPAR-γ agonism. The receptor’s transcriptional activity is dose-dependent, and suboptimal dosing may result in incomplete transrepression of inflammatory cytokines, thereby negating the very therapeutic rationale for its use. Furthermore, the assertion that thiazide diuretics reduce edema by 38% is statistically misleading without clarification of the confidence intervals, which were not reported in the referenced observational study. One must interrogate the methodology - was there adjustment for baseline eGFR? For concomitant insulin use? For dietary sodium intake? The answer, predictably, is no.
Ashley Bliss
December 26, 2025 AT 16:20
I used to think medicine was about healing. Now I just see a series of compromises. You take a pill to fix your blood sugar, but then your legs turn into water balloons. You take another pill to fix that, and now your potassium is in the toilet. You switch to a GLP-1, and suddenly you can’t keep anything down - not even your dignity. We’re not treating disease anymore. We’re playing whack-a-mole with our own bodies. And the worst part? The doctors are just as tired as we are. They’re just signing prescriptions because they don’t have time to listen. And we’re just numb. We’ve stopped asking, "Is this really helping?" and started asking, "How do I survive this?"
Connie Zehner
December 27, 2025 AT 01:12
I gained 12 lbs in 3 weeks on pioglitazone and my doctor just said "it's normal" 😭 I cried in the pharmacy parking lot. Then I found a Reddit group of 300 people who all had the same thing. Nobody warned me. I feel so violated. Also, I think Big Pharma is hiding that TZDs make you crave carbs. I ate 3 pizzas in one night and I didn't even want to. It was like my brain got hacked. I'm now on metformin and I'm crying happy tears. Also, if you're on this drug, check your urine. If it's really dark, you're drowning. I swear.
holly Sinclair
December 28, 2025 AT 22:43
There’s something deeply philosophical about how we treat chronic illness in modern medicine - we don’t seek harmony, we seek control. We layer drugs on top of drugs like we’re building a tower of Band-Aids over a collapsing foundation. TZDs work because they force cells to respond to insulin - but they don’t fix why the cells stopped responding in the first place. Is it the sugar? The stress? The sedentary life? The gut microbiome? We treat the symptom, not the silence. The swelling isn’t just fluid - it’s the body screaming that something’s fundamentally out of alignment. Maybe the real solution isn’t a new drug, but a return to rhythm: movement, sleep, food as medicine, community. We’ve outsourced healing to pills because we’ve forgotten how to listen to our own bodies. And now we’re surprised when they rebel.