Relationships and Health: How Medicine, Money and Communication Shape Care
Your relationships change how you take medicine, how you pay for it, and how you feel day to day. Partners, family members, doctors and pharmacists all influence whether treatment helps or causes stress. When everyone communicates, care improves. When they don’t, mistakes happen and trust can break.
Talk about meds with the people closest to you
Start by naming who helps you. A partner might remind you to take a pill, a friend might drive you to appointments, or an adult child might manage refills. Be specific when you talk: share dose times, side effects to watch for, and what symptoms need a doctor. If a drug is changing your mood, sleep or sex drive, say so plainly. Those issues affect the relationship as much as the illness.
Keep one shared list of medications with names, doses, and why each drug is taken. Bring that list to every appointment. It prevents double-dosing and makes switching drugs smoother—whether it’s moving off Metformin, choosing a carvedilol substitute, or trying a different inhaler. If your doctor suggests a substitute, explain the plan to your partner so they can help notice benefits or side effects.
Use pharmacies, discounts and online tools wisely
Money often strains relationships. Prescription costs lead people to skip doses or argue. Look into discount tools and coupon services, but compare them first. Some services genuinely cut bills; some look cheap and carry risk. When ordering online, choose pharmacies that require a prescription, show a physical address and list a pharmacist phone number.
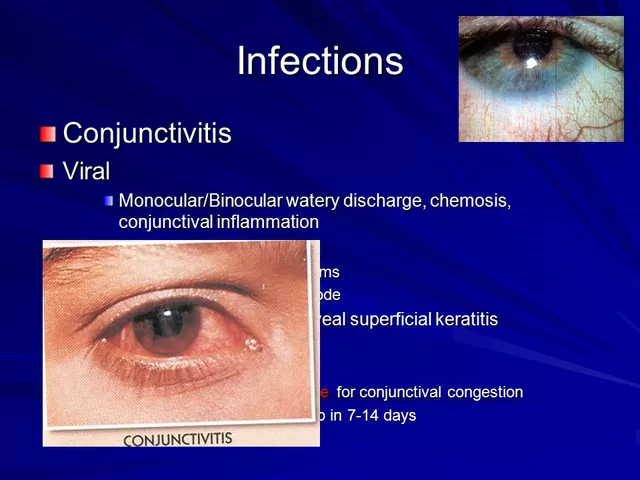
Watch for clear warning signs: extremely low prices with no prescription, no pharmacist contact, or vague shipping info. If you’re unsure about a site, ask your pharmacist or doctor. They can suggest licensed alternatives and check for drug interactions—important when you mix antibiotics, heart meds, or antidepressants.
When a pharmacist recommends a cheaper alternative or an equivalent inhaler, ask for a short explanation: how it works, what to expect, and any monitoring needed. That keeps everyone on the same page and avoids surprises that can damage trust between partners or caregivers.
Set simple rules for emergencies and privacy. Agree who calls the doctor, who manages refills, and who can access online accounts. Store medicines safely and use shared calendars or reminders so missed doses don’t become a pattern. Celebrate small wins when a treatment reduces symptoms—positive feedback helps partners stay supportive.
If mental health or eating disorders are part of your story, include trusted family members in care plans only with consent. Medications like prochlorperazine may be part of a broader approach; open, honest talks between patient, clinician and supporter make treatment safer and more effective.
Small, concrete steps—clear lists, direct talks, safe pharmacy choices, and shared emergency plans—cut confusion and keep relationships working for your health.