Hormonal imbalance: how to spot it and what to do
Hormones control your mood, energy, weight, sleep and sex drive. When they’re out of balance you notice real, everyday problems — fatigue, odd weight changes, irregular periods, acne, mood swings or low libido. This page helps you recognize common signs, understand likely causes, and take practical first steps so you can get answers fast.
Common signs and likely causes
Here are clear symptom groups that often point to a hormonal issue:
- Energy and sleep: constant tiredness, trouble falling asleep, or waking up exhausted can indicate thyroid problems or cortisol (stress hormone) issues.
- Weight and appetite: sudden weight gain or loss, stubborn belly fat, or increased appetite despite no obvious reason — think insulin resistance, thyroid or sex-hormone changes.
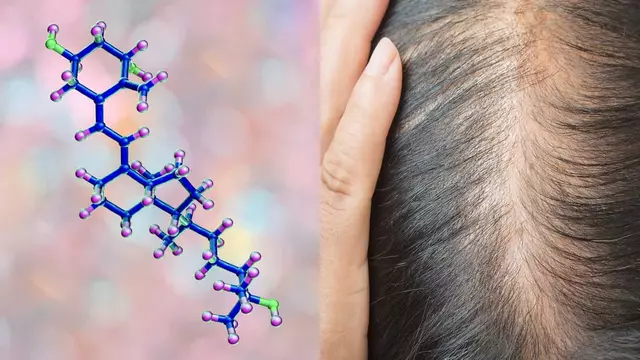
- Reproductive and skin changes: irregular or missing periods, heavy bleeding, acne, excess facial hair, or low libido often relate to estrogen, progesterone or androgen imbalances. In people on birth control, symptoms can shift when stopping or switching pills.
- Mood and cognition: anxiety, depression, brain fog, or memory slips can be connected to thyroid dysfunction, menopause transitions, or chronic stress affecting cortisol.
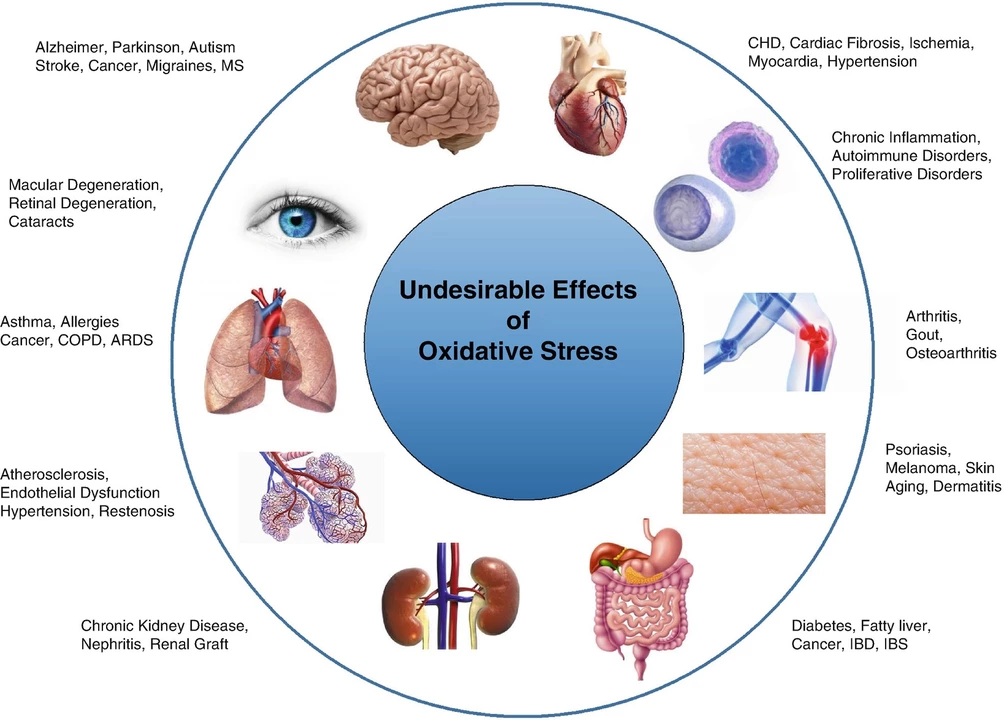
Common causes include thyroid disease, polycystic ovary syndrome (PCOS), menopause or perimenopause, prolonged stress, poor sleep, certain medications, rapid weight change, and chronic illness. Age and genetics also play a role.
What to do next — tests and simple fixes
Step 1: track symptoms. Keep a short daily log for 2–4 weeks: sleep, mood, periods, energy, weight changes, medications and meals. That makes your visit more useful.
Step 2: see your primary care doctor or gynecologist. Describe the pattern, show your log, and ask for baseline blood tests. Typical labs: TSH and free T4 (thyroid), fasting glucose and HbA1c (blood sugar), fasting insulin if available, morning cortisol if suspected, and sex hormones (estradiol, progesterone, testosterone) timed to your cycle if relevant.
Step 3: simple lifestyle fixes that help most hormone issues—sleep 7–9 hours, reduce sugar and refined carbs, move 30 minutes most days (mix walking and strength), manage stress with short breathing breaks or a 10-minute walk, and avoid smoking and heavy alcohol use. These steps improve insulin and cortisol balance and often reduce symptoms quickly.
Medications and procedures: your doctor may prescribe thyroid hormone, birth-control pills or progesterone for cycle issues, metformin for PCOS or insulin resistance, or referral for hormone replacement if you’re in menopause. Don’t self-prescribe. Discuss risks and benefits with your clinician.
When to get urgent help: sudden fast heart rate, fainting, severe unexplained weight loss, extreme weakness, or very high blood sugar need urgent evaluation.
If symptoms persist after basic care, ask for a referral to an endocrinologist. That specialist can run advanced tests and design a tailored plan. You don’t have to accept feeling ‘off’—with the right steps most people see real improvement.