Cancer Rehabilitation: Your Roadmap to Recovery
When talking about cancer rehabilitation, a coordinated set of services that help survivors regain function, manage side effects, and improve quality of life. Also known as oncology rehab, it brings together doctors, therapists, dietitians, and mental‑health professionals to address the whole person, not just the disease. Cancer rehabilitation is built on three core ideas: assess the lingering impacts of treatment, design a personalized plan, and monitor progress over time.
Physical Therapy: Moving Past Treatment Fatigue
One of the first pillars of recovery is physical therapy, targeted exercise programs that restore strength, balance, and endurance after surgery, chemotherapy, or radiation. Physical therapy encompasses activities like gentle stretching, resistance training, and cardio conditioning, all tailored to an individual's stamina. Studies show that patients who start a structured PT program within weeks of treatment report less fatigue, better mobility, and a quicker return to daily chores. Therapists also teach safe movement techniques to protect incisions and reduce lymphedema risk.
Beyond the gym, PT teams often coordinate with occupational therapists to adapt home environments—installing grab bars, recommending ergonomic tools, and teaching energy‑conservation strategies. This integrated approach requires ongoing communication between clinicians, ensuring that exercise intensity matches healing progress and that any new side effects are addressed promptly.
Nutritional Support: Fueling Healing from the Inside
Another critical component is nutritional support, personalized diet plans that help cancer survivors maintain weight, preserve muscle mass, and boost immunity. Malnutrition is common after aggressive therapy, and a tailored nutrition strategy can reduce infection risk and improve wound healing. Dietitians often recommend high‑protein foods, omega‑3 rich fish, and antioxidant‑packed fruits and veggies to combat oxidative stress.
Supplement choices matter, too—some patients benefit from vitamin D, calcium, or iron, while others need to avoid certain herbs that could interfere with chemotherapy metabolism. The diet plan is usually adjusted as treatment cycles change, making it a dynamic element of the rehab process. Good nutrition also supports the effectiveness of medications discussed later, like antidepressants or pain relievers, by ensuring proper absorption and reducing side‑effects.
Psychological Counseling: Coping with the Emotional Aftermath
Emotional well‑being gets a spotlight through psychological counseling, structured therapy that addresses anxiety, depression, and post‑traumatic stress after a cancer diagnosis. Counseling influences overall recovery because mental health directly impacts adherence to medication and participation in PT or nutrition programs. Techniques range from cognitive‑behavioral therapy to mindfulness‑based stress reduction, each chosen based on the survivor's preferences.
When counseling identifies clinical depression, clinicians may prescribe antidepressants such as sertraline (Zoloft) or bupropion (Wellbutrin), which appear in many of our medication guides. Proper pharmacologic management, in turn, can lift mood, improve sleep, and give patients the energy needed for rehab activities. The synergy between therapy and medication illustrates why a multidisciplinary team is essential.
Pharmacologic Management: Managing Pain, Fatigue, and Other Symptoms
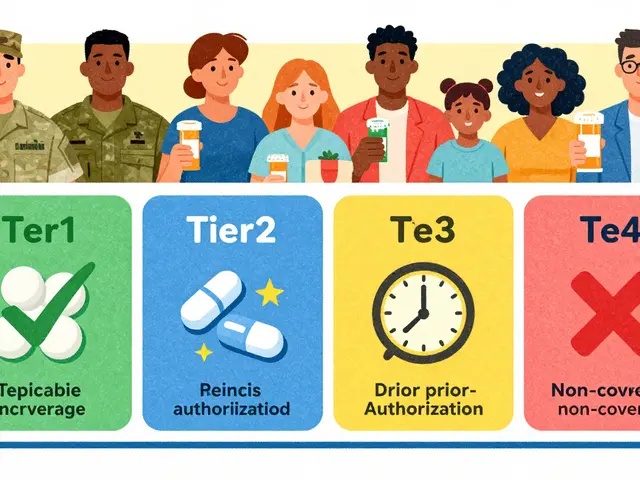
The final piece is pharmacologic management, the careful selection and monitoring of drugs to control pain, nausea, fatigue, and mental‑health symptoms during cancer recovery. This may include opioid‑sparing analgesics, anti‑emetics, or drugs for neuropathic pain like gabapentin. Each medication is matched to the survivor’s specific side‑effect profile, with regular reviews to adjust dosage or switch agents if needed.
Because many of these drugs have interactions with nutrition or exercise, clinicians coordinate with dietitians and physical therapists to avoid conflicts—for example, timing pain medication so it doesn’t mask warning signs during a PT session. The goal is a balanced regimen that maximizes relief while minimizing adverse effects, allowing the survivor to stay active in all other rehab domains.
Together, these four pillars—physical therapy, nutritional support, psychological counseling, and pharmacologic management—form a cohesive cancer rehabilitation ecosystem. Below you’ll find a curated set of articles that dive deeper into each area, from drug‑specific buying guides to practical tips for staying fit after treatment. Explore the collection to build your personalized recovery plan and keep moving forward with confidence.