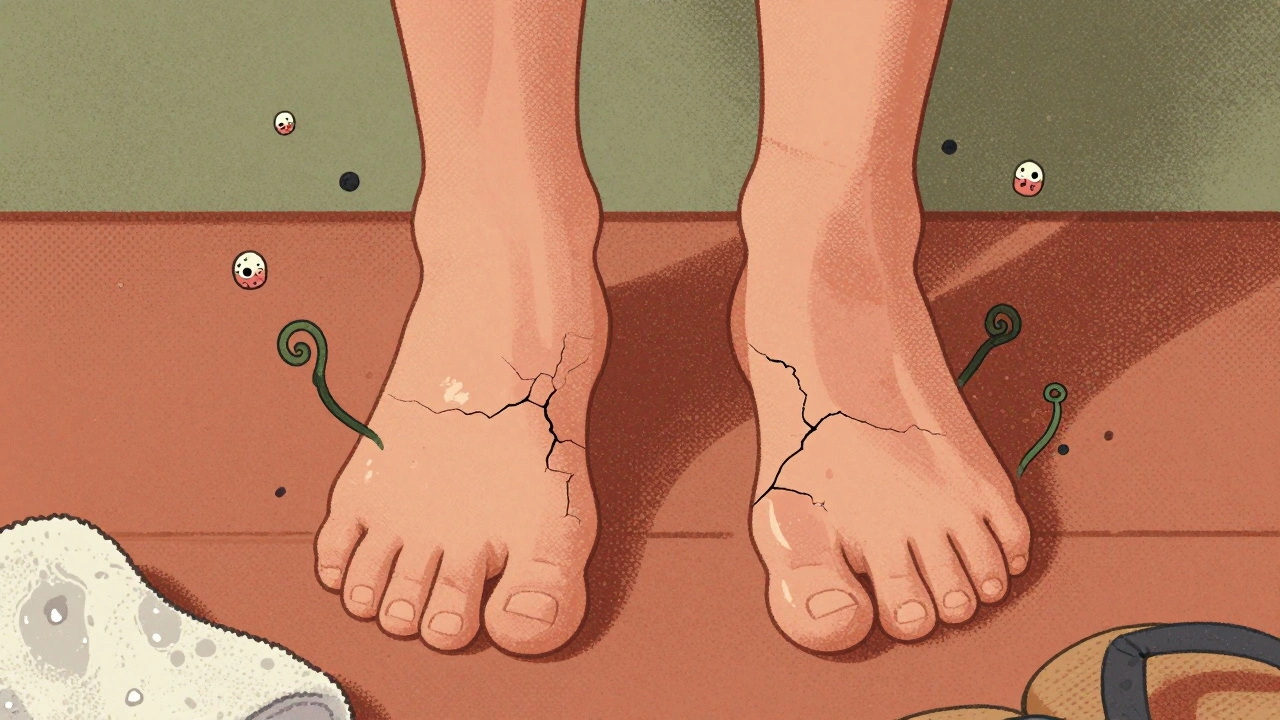
Ever had that itchy, peeling skin between your toes that won’t go away no matter how much you scrub? Or maybe you’ve dealt with a stubborn white coating in your mouth that feels like cotton? These aren’t just annoyances-they’re fungal infections, and they’re way more common than most people realize. Around 15% of the global population has a fungal skin infection at any given time. In warm, humid places like Perth, that number can jump to 30%. The two biggest culprits? Athlete’s foot and Candida. They’re not the same thing, and they don’t get treated the same way. But most people treat them like they are.
What’s Actually Growing on Your Skin?
Not all fungi are the same. Athlete’s foot is caused by dermatophytes-fungi that live for one thing: keratin. That’s the tough protein in your skin, hair, and nails. These fungi don’t care about your blood or organs. They just want to eat the outer layer of your feet, especially between your toes where it’s warm, damp, and dark. The usual suspects? Trichophyton rubrum, T. mentagrophytes, and Epidermophyton floccosum. You pick them up from locker room floors, public showers, or even sharing a towel. Candida, on the other hand, is a yeast. Most of us carry it naturally-in our mouths, guts, and vaginal areas. It’s harmless until something tips the balance. Antibiotics, diabetes, a weak immune system, or even just wearing sweaty socks for days can let it overgrow. When it does, it’s not just skin-deep. It can cause vaginal yeast infections (affecting 75% of women at least once), oral thrush, or even spread into the bloodstream in severe cases. That’s when it gets dangerous.How Athlete’s Foot Shows Up (And How to Spot It)
Athlete’s foot doesn’t look the same on everyone. There are three main types:- Interdigital (70% of cases): This is the classic peeling, cracking skin between the fourth and fifth toes. It itches, burns, and sometimes smells. The skin gets soggy and white from moisture.
- Moccasin type (20%): This one sneaks up. It starts as dry, flaky skin on the soles and sides of your feet. Looks like bad dry skin-until you realize it won’t improve with lotion.
- Vesicular/bullous (10%): Small blisters appear suddenly. These can burst, leaving raw, painful patches. Often mistaken for a reaction to shoes or socks.
Candida: More Than Just a Yeast Infection
Candida albicans is the usual offender. But unlike athlete’s foot, it doesn’t need a public shower to thrive. It grows when your body’s natural balance is off. Antibiotics kill off good bacteria that keep yeast in check. Diabetes means more sugar in your system-yeast loves sugar. Steroids or chemotherapy? That weakens your immune system’s ability to say “no.” Symptoms vary by location:- Vaginal: Thick, white discharge (like cottage cheese), intense itching, burning during urination or sex.
- Oral (thrush): White patches on the tongue or inside cheeks that won’t scrape off. Pain, loss of taste, cracking at the corners of the mouth.
- Skin folds: Red, itchy rash in armpits, under breasts, or in the groin. Often mistaken for heat rash.
- Invasive: Fever, chills, low blood pressure. This is rare-but deadly. About 40% of people with invasive candidiasis don’t survive if it’s not treated fast.

Antifungal Treatments: What Works, What Doesn’t
You’ve probably seen shelves full of antifungal creams. But not all are created equal. Here’s what actually clears up these infections:For Athlete’s Foot:
- Terbinafine (Lamisil): The gold standard. Kills fungi, doesn’t just slow them down. Works in 1-2 weeks for most people. One study showed 78% of users saw improvement in under a week.
- Clotrimazole or Miconazole: Common OTC options. Slower. Takes 4-6 weeks. Good for mild cases, but recurrence is high if you stop too soon.
- Whitfield’s Ointment: A mix of benzoic acid and salicylic acid. Not just antifungal-it peels off dead skin. Great for the peeling, cracked type. Studies show 65% clearance at 4 weeks-better than clotrimazole alone.
For Candida:
- Topical: Clotrimazole or miconazole creams or suppositories for vaginal infections. Nystatin mouthwash for thrush.
- Oral: Fluconazole (Diflucan). One pill often clears up a vaginal infection. For recurrent cases, doctors may prescribe weekly doses for months.
- New option: Ibrexafungerp (Brexafemme). Approved in 2021, it’s the first new class of antifungal in 20 years. Works for stubborn vaginal yeast infections that don’t respond to fluconazole.
Why Treatments Fail (And How to Avoid It)
Most people aren’t failing because the medicine doesn’t work. They fail because they don’t treat the environment.- Wearing the same socks: Fungi live in fabric. Change socks daily. Use cotton or moisture-wicking blends.
- Not drying feet properly: After a shower, use a separate towel for your feet. Dry between your toes like you’re drying a baby’s skin.
- Walking barefoot: Locker rooms, pools, hotel bathrooms? Wear flip-flops. Even if you think you’re clean, you’re not.
- Sharing shoes or towels: That’s how you spread it-and catch it.
- Ignoring moisture: If your feet stay damp, use antifungal powder. A 2% miconazole powder can help where creams can’t reach.

When to See a Doctor
You don’t need to see a doctor for every itchy toe. But if any of these happen, get help:- Your skin is cracked, bleeding, or oozing pus.
- You have fever, swelling, or red streaks up your leg.
- You have diabetes and any foot issue-even mild.
- It keeps coming back after treatment.
- Oral thrush won’t go away after 2 weeks of treatment.
What’s New in 2025?
Science isn’t standing still. In March 2023, a new topical antifungal called olorofim showed 82% cure rates for stubborn athlete’s foot that didn’t respond to anything else. It’s still in trials, but it’s a big deal. The CDC’s “My Action Plan” program, rolled out in 2022, helped diabetes clinics cut recurrent fungal infections by 35% by teaching patients daily foot checks and moisture control. That’s real progress. But here’s the warning: a new strain of athlete’s foot fungus, Trichophyton indotineae, has spread from India to 28 countries. It’s resistant to common antifungals. The WHO lists it as a priority pathogen. We’re heading toward a time when some infections won’t respond to old treatments.Bottom Line: Treat It Right
Fungal infections aren’t embarrassing. They’re common, treatable, and preventable. But you can’t treat them like a cold. You need the right medicine, applied correctly, for long enough. And you need to fix the conditions that let them grow.- Use terbinafine for athlete’s foot-it’s faster and more reliable.
- Don’t stop antifungal treatment early, even if it feels better.
- Keep feet dry, change socks daily, wear flip-flops in public showers.
- If you have diabetes, check your feet every day.
- For recurrent yeast infections, talk to your doctor about underlying causes.
Lara Tobin
December 14, 2025 AT 10:19
I had athlete’s foot for months and thought it was just dry skin... until I started using terbinafine and it vanished in 10 days. 🙌 Don’t stop when it stops itching - that’s when the real battle begins.
Keasha Trawick
December 15, 2025 AT 03:32
Fungi are the silent saboteurs of modern hygiene culture. Dermatophytes don’t care about your ‘clean living’ Instagram aesthetic - they thrive in the damp, dark corners of your life. Candida? That’s your gut screaming for balance. Antibiotics are the Trojan horse, sugar is the bait, and your immune system is the guard who fell asleep. This isn’t a rash. It’s a microbiome civil war.
Bruno Janssen
December 16, 2025 AT 17:45
I hate how people treat this like it’s no big deal. I got thrush after antibiotics and felt like my mouth was full of cotton balls coated in chalk. No one gets it unless they’ve been there.
Scott Butler
December 17, 2025 AT 10:38
This is why America’s hygiene standards are falling apart. Back in my day, we didn’t need fancy antifungals - we just washed our feet and didn’t walk around barefoot in public. Problem solved. Now everyone’s blaming the fungus instead of their laziness.
Deborah Andrich
December 18, 2025 AT 04:18
I’m a nurse and I’ve seen people ignore foot infections until they end up in the ER with cellulitis. Please don’t be that person. Dry your toes. Wear flip-flops. Use the cream for two weeks after it feels better. It’s not complicated. Your feet will thank you.
Richard Ayres
December 19, 2025 AT 07:20
The data presented here is both clinically accurate and remarkably accessible. It’s refreshing to see a piece that bridges the gap between medical literature and public understanding. The emphasis on environmental factors - socks, towels, moisture control - is not merely anecdotal but evidence-based and often overlooked in patient education.
Rawlson King
December 20, 2025 AT 10:53
You people treat fungus like it’s a glitch in your life. In Canada, we don’t mess around. If your feet are peeling, you go to the pharmacy, get terbinafine, and you don’t come back until it’s gone. No excuses. No ‘maybe it’ll clear up.’ Fungus doesn’t care about your feelings.
kevin moranga
December 20, 2025 AT 17:39
I used to think I was just bad at foot care until I found out I was sharing towels with my roommate. Once I switched to cotton socks, dried my toes like they were newborns, and started using miconazole powder every morning? No more itch. No more shame. It’s not magic - it’s consistency. You don’t need a PhD to beat fungus. You just need to be boringly disciplined.
Alvin Montanez
December 22, 2025 AT 16:37
I don’t know why people are so shocked by this. Candida overgrowth? That’s what happens when you eat sugar like it’s candy and take antibiotics like they’re vitamins. You want to fix it? Stop eating donuts. Stop being lazy. Stop blaming the fungus. You created this. Your body is not a petri dish for your bad habits.
Cole Newman
December 23, 2025 AT 20:06
Wait - so you’re telling me I can’t just use tea tree oil and hope for the best? I’ve been doing that for months. My toes still look like they’re shedding snake skin. And now you say I need to use actual medicine? For two WEEKS after it feels better? Bro. That’s a lot of effort.
Casey Mellish
December 24, 2025 AT 15:58
As an Aussie, I’ve seen more athlete’s foot than kangaroos in the outback. We call it ‘tinea’ here - and yeah, it’s everywhere. But here’s the secret: Australian tea tree oil works wonders as a supplement. Not a cure, but it kills the smell and cools the burn. Combine it with terbinafine? You’re basically untouchable.
Tyrone Marshall
December 26, 2025 AT 09:33
The real tragedy isn’t the infection - it’s how we’ve normalized suffering. We accept itchy feet, yeast infections, and thrush as ‘just part of being human.’ But they’re not. They’re signals. Your body is begging you to change your habits. Fungi don’t invade. They’re invited. The cure isn’t just in the cream - it’s in your socks, your diet, your shower routine, your silence around your own health.
Emily Haworth
December 27, 2025 AT 09:18
I’m not saying this is a government plot... but why is it only in the last 10 years that everyone suddenly has fungus? 🤔 Coincidence? Or did they add something to the water? Or the shoes? Or the laundry detergent? I’ve seen people with thrush who’ve never taken antibiotics. Something’s off. And I’m not the only one who noticed. 👁️🗨️ #FungusGate
Tom Zerkoff
December 28, 2025 AT 20:02
The clinical efficacy of terbinafine versus azoles in dermatophytosis is well-documented in multiple randomized controlled trials, including the 2018 Cochrane review. The persistence of recurrence rates above 40% is directly correlated with suboptimal treatment duration and non-adherence to hygiene protocols. It is not a failure of pharmacology - it is a failure of behavioral compliance. This is not a medical issue. It is a public health education crisis.