Asthma treatment options: inhalers, pills, biologics and smart steps
If your breathing gets tight or you cough a lot, knowing your asthma treatment options makes a big difference. Treatments fall into quick-relief (reliever) and long-term control (controller) categories. Pick the right mix with your doctor, and focus on how you use the medicine—technique matters more than you think.
Immediate relief vs daily control
For sudden symptoms, short-acting beta-agonist inhalers (SABA) like salbutamol give fast relief within minutes. Keep one handy, but don’t rely on it alone. Needing it often means your controller plan needs attention. For everyday control, inhaled corticosteroids (ICS) are the foundation. They lower airway inflammation and reduce flare-ups. Many people use combination inhalers that include an ICS plus a long-acting bronchodilator (LABA). These combo inhalers simplify treatment and keep symptoms down with once- or twice-daily use.
Other inhaler options include long-acting muscarinic antagonists (LAMA) such as tiotropium, usually added when ICS/LABA isn’t enough. Dry powder devices and metered-dose inhalers work differently. If your inhaler technique is off, a spacer can help get medicine into your lungs instead of your mouth.
Oral meds, shots, and lifestyle steps
Some people add oral medicines like leukotriene receptor antagonists (montelukast) for allergy-linked asthma or mild persistent symptoms. Short courses of oral steroids help during severe flare-ups but aren’t safe for long-term use because of side effects like weight gain, mood changes, and bone loss.
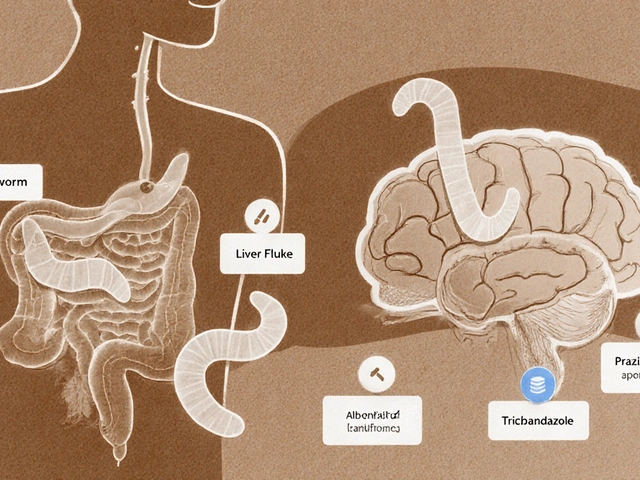
For moderate-to-severe asthma that doesn’t respond to standard treatment, biologic injections target the immune drivers behind attacks. Drugs such as anti-IgE or anti-IL5 therapies can cut down exacerbations and steroid need. These require specialist assessment and testing for blood markers or allergy triggers.
Simple non-drug moves also pay off: avoid known triggers (smoke, strong smells, cold air where possible), treat allergic rhinitis, keep vaccines up to date, and get a written asthma action plan. Track peak flow or symptoms so you can tell when to step up treatment early.
Finally, don’t guess about doses or medication swaps. Ask your clinician about generic options, inhaler equivalents (for example, if you read about Symbicort alternatives), and safe online pharmacy choices if cost is an issue. Check technique in the clinic, review your plan yearly, and speak up if you’re using rescue inhalers more than twice a week.
Got frequent flare-ups or morning cough? Book a review with your doctor or asthma nurse. Small changes in medicines or how you use them often mean much better days and fewer emergency visits.