Antibiotic: Practical Guide to Uses, Safety, and Buying Online
Antibiotics treat bacterial infections — not colds or most sore throats. Knowing when and how to use them keeps you safe and slows resistance.
What are antibiotics? They are drugs that kill bacteria or stop them from growing. Common types include penicillins, cephalosporins, macrolides, and fluoroquinolones. Doctors pick one based on the infection, allergy history, and local resistance patterns.
When should you take antibiotics?
Only when a bacterial infection is likely. If your doctor confirms strep throat, a urinary tract infection, or certain skin infections, antibiotics help. Viral illnesses like the flu, most coughs, and many sore throats do not need them. If symptoms are mild, ask your clinician about watchful waiting or testing before starting meds.
Finish the prescribed course unless your doctor tells you otherwise. Stopping early can leave surviving bacteria that are harder to treat. If you get side effects like severe diarrhea, rash, or breathing problems, stop and get medical help.
Buying antibiotics online safely
Can you buy antibiotics online? Yes — but do it carefully. Use a licensed online pharmacy that requires a prescription and shows a physical address and pharmacist contacts. Avoid sites that sell prescription drugs without asking for a prescription or that offer unusually low prices with no verifiable details.
Check reviews from independent sources, confirm the pharmacy is registered in your country, and look for secure payment and clear shipping policies. If you must order internationally, factor in customs delays and proper storage during transit, especially for temperature-sensitive products.
Generic versions are often cheaper and work the same as brand-name drugs. Ask your prescriber or pharmacist if a generic is appropriate. Never share antibiotics with others or use leftover pills for a new illness.
Worried about resistance? Use antibiotics only when needed, follow dosing instructions, and avoid pressuring clinicians for antibiotics when they say no. Vaccines, handwashing, wound care, and safe food handling reduce the need for antibiotics in the first place.
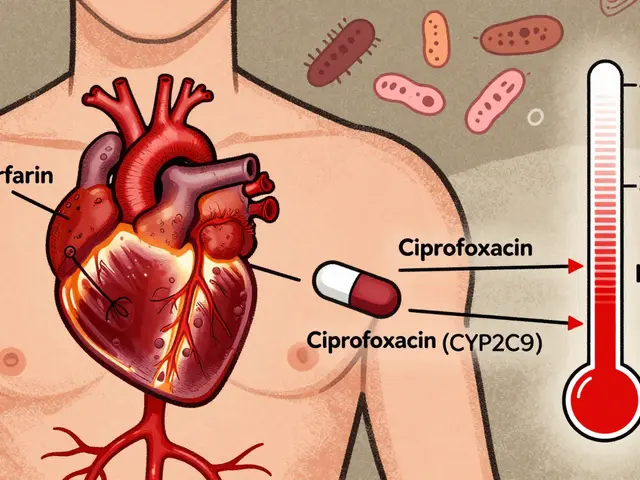
Some antibiotics interact with other medicines or foods. Antacids, calcium, magnesium, and iron can reduce absorption of tetracyclines and fluoroquinolones. Also tell your doctor if you take blood thinners, diabetes drugs, or statins — interactions can change how drugs work. Avoid alcohol with metronidazole or tinidazole; mixing them can cause severe nausea, flushing, and rapid heart rate.
Store antibiotics in original packaging and follow temperature instructions. Don't use expired pills. Return unused meds to pharmacy take-back programs or follow local disposal rules — never share leftovers.
If you suspect you're allergic to penicillin, ask about allergy testing — many people who think they're allergic can safely take penicillins after testing. If symptoms fail to improve in 48–72 hours, call your clinician for reassessment; you may need a different antibiotic or additional tests.
Keep updated medication list for appointments.