Every year, over 1 million people in the U.S. end up in emergency rooms because of harmful reactions to medications. Many of these aren’t accidents-they’re preventable. Adverse drug events (ADEs) are one of the biggest threats to patient safety today, yet most people don’t know what they are or how to protect themselves. This isn’t just a hospital problem. It happens in doctor’s offices, pharmacies, and right at home.
What Exactly Is an Adverse Drug Event?
An adverse drug event isn’t just a side effect. It’s any injury caused by taking a medication-whether it’s because of a mistake, a reaction, or even just taking too much. The key difference? An ADE is harm that actually happened to a patient. Not just a risk. Not just a warning. Real damage.
Think of it this way: if you take your blood pressure pill and your blood pressure drops too low, making you dizzy and fall, that’s an ADE. If your doctor prescribes two drugs that cancel each other out, and you end up in the hospital, that’s an ADE. If you accidentally take double your insulin dose and go into hypoglycemia-that’s an ADE too.
The Institute of Medicine first brought this issue to light in 2000, showing that medication errors alone were killing at least 7,000 people a year in U.S. hospitals. Since then, we’ve learned that ADEs are behind 125,000 hospital admissions and 1 million ER visits every year in the U.S. alone. And the worst part? Nearly half of them could have been avoided.
The Five Main Types of Adverse Drug Events
Not all ADEs are the same. They fall into five clear categories, each with different causes and risks.
- Adverse Drug Reactions (ADRs): These are the body’s unexpected or harmful response to a drug at normal doses. Think rashes, liver damage, or severe dizziness. About 80% of these are Type A reactions-predictable, dose-related, and often preventable with better monitoring.
- Medication Errors: These happen when something goes wrong in prescribing, dispensing, or taking the medicine. A nurse gives the wrong dose. A pharmacist misreads the handwriting. You take your pill at the wrong time. These aren’t rare. They’re the most common cause of ADEs.
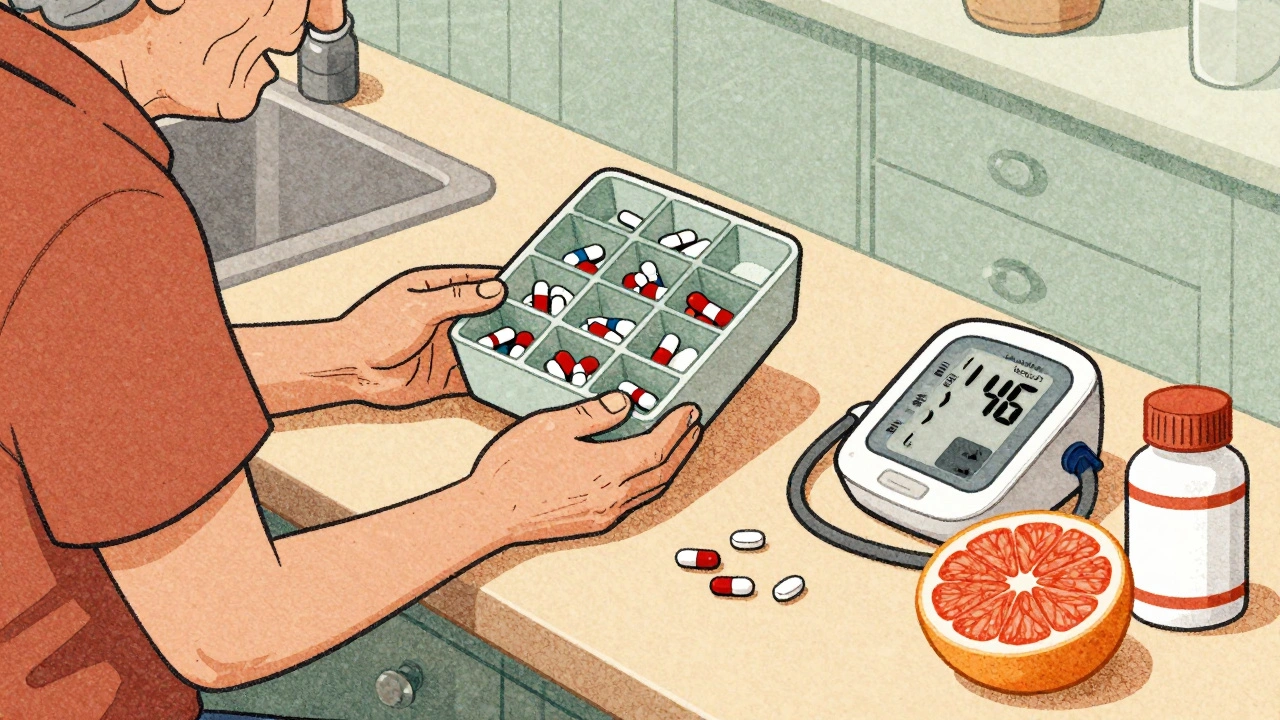
- Drug-Drug Interactions: When two or more medications mix and create a dangerous effect. Warfarin and certain antibiotics? Big risk. Statins and grapefruit juice? Can cause muscle damage. Over 40% of older adults take five or more medications, making interactions almost inevitable without careful review.
- Drug-Food Interactions: Food can change how your body absorbs or breaks down a drug. Antidepressants and aged cheese? Can spike blood pressure. Tetracycline and dairy? Blocks absorption. These are often overlooked because they seem harmless-until they’re not.
- Overdoses: Whether accidental or intentional, too much of a drug can be deadly. Opioids are the biggest concern here. In 2021, over 70,000 deaths in the U.S. were linked to synthetic opioids like fentanyl. Even a small miscalculation in insulin or anticoagulant dosing can lead to emergency hospitalization.
Some reactions are rare and unpredictable-called Type B reactions. These aren’t caused by dose. They’re tied to your genes, your immune system, or unknown factors. But the majority? Type A. They’re predictable. And that means they’re preventable.
The Top Three High-Risk Medications
Not all drugs carry the same risk. Three classes stand out as the most dangerous-and the most preventable.
1. Anticoagulants (like warfarin)
Warfarin is the single most common drug linked to ADE-related hospital admissions. Why? It has a narrow therapeutic window-too little, and you clot; too much, and you bleed. Thirty-three percent of all ADEs in hospitals come from anticoagulants. Outpatient monitoring is often poor: in 35% of cases, patients’ INR levels (the test that measures blood thinning) are outside the safe range. That’s not just a lab result-it’s a ticking time bomb.
2. Diabetes Medications (especially insulin)
Insulin saves lives-but it’s also one of the most dangerous drugs if misused. Around 100,000 emergency visits each year are due to insulin-related hypoglycemia. Sixty percent of those patients are over 65. Many don’t know how to adjust their dose when they eat less or exercise more. Some use outdated pens or misread the numbers. A simple mistake can lead to seizures, coma, or death.
3. Opioids
Opioids are responsible for 40% of all medication-related deaths. Fentanyl, in particular, is 50 to 100 times stronger than morphine. A tiny miscalculation-like a 2 mg dose instead of 1 mg-can be fatal. Even after surgery, patients are often sent home with more pills than they need. Unused pills sit in medicine cabinets, where kids or elderly relatives might find them. Or worse, they get sold or misused.

How to Prevent Adverse Drug Events
Preventing ADEs isn’t just the job of doctors and pharmacists. It’s a team effort-and you’re part of the team.
- Keep a complete, up-to-date medication list. Include every pill, patch, vitamin, herb, and supplement. Bring it to every appointment. A 2019 JAMA study found that just reviewing this list cuts ADE risk by 30%.
- Ask: “Why am I taking this?” If your doctor prescribes something new, ask: Is this really needed? Are there safer alternatives? Can I stop something else? The Canadian Deprescribing Guidelines show that checking for unnecessary prescriptions prevents 23% of inappropriate ones.
- Use pharmacy tools. Most pharmacies now have systems that flag dangerous interactions. Ask your pharmacist to run a check every time you pick up a new prescription. Tools like Lexicomp catch 15% of high-risk interactions before they happen.
- Get medication reconciliation. This is when your care team compares your current meds to what you were taking before a hospital stay or clinic visit. Done right, it reduces post-discharge ADEs by 47%. Make sure it happens every time you’re discharged.
- Understand your meds. Don’t just take them. Know the name, the dose, why you’re taking it, and what to watch for. A Cochrane review found that patients who get clear education are 22% more likely to take their meds correctly-and 22% less likely to have an ADE.
- Use electronic prescribing. Handwritten prescriptions are a major source of error. E-prescribing cuts mistakes by 48%. If your doctor still writes scripts by hand, ask if they can switch to digital.
Pharmacists are your secret weapon. Medication Therapy Management (MTM) services-where pharmacists sit down with you to review everything you take-find an average of 4.2 medication problems per patient. That’s 32% fewer ADEs. Yet only 15% of people in the U.S. use these services. You don’t need a referral. Ask your pharmacy.
Technology Is Changing the Game
Tools are getting smarter. The Veterans Affairs system uses real-time dashboards that alert doctors if a patient’s warfarin dose is putting them at risk. They’ve cut bleeding events by 28%. Some hospitals now use pharmacogenomic testing-checking your genes before prescribing certain drugs. For example, some people can’t process clopidogrel (a blood thinner) properly. Testing for that gene reduces ADEs by 35%.
Artificial intelligence is next. Johns Hopkins ran a pilot using machine learning to analyze 50+ patient factors-age, kidney function, other meds, lab results-and predicted who was most likely to have an ADE. The result? A 17% drop in preventable events. These tools aren’t science fiction-they’re already in use.
But here’s the catch: 89% of U.S. hospitals have electronic records, but only 45% have smart alerts for high-risk drugs. We have the tech. We just need to use it.

What’s Still Holding Us Back?
Even with all the tools and data, progress is slow. Why?
One big reason: deprescribing. Many older adults are on drugs they don’t need anymore-anticholinergics for sleep, benzodiazepines for anxiety. These increase fall risk, confusion, and dementia. The VA’s deprescribing program cut ADEs from these drugs by 40%. But only 15% of primary care doctors regularly screen for inappropriate meds, even though the Beers Criteria (a trusted guide) has been around for years.
Another problem: communication gaps. A pharmacist catches a dangerous interaction, but the doctor never sees the note. A patient forgets to mention they’re taking turmeric for arthritis-and it interferes with their blood thinner. These aren’t failures of technology. They’re failures of teamwork.
And then there’s cost. Pharmacogenomic testing is still expensive and not covered by most insurance. Only 5% of patients get tested today. But by 2027, that number could hit 30%. When it does, we could prevent over 100,000 ADEs a year just by matching the right drug to the right gene.
What You Can Do Today
You don’t need to wait for policy changes or new tech. Here’s what you can do right now:
- Write down every medication you take-including over-the-counter pills and supplements.
- Take that list to every doctor visit. Ask: “Is this still necessary?”
- Ask your pharmacist to check for interactions every time you pick up a new prescription.
- If you’re on warfarin, insulin, or an opioid, ask if you need more frequent monitoring.
- Don’t be afraid to ask questions. If you don’t understand why you’re taking something, say so.
Medication safety isn’t about being perfect. It’s about being aware. It’s about asking for help. It’s about speaking up when something doesn’t feel right.
Every year, hundreds of thousands of people are hurt by drugs that shouldn’t have harmed them. It doesn’t have to be that way. You have more power than you think.
What’s the difference between an adverse drug reaction and an adverse drug event?
An adverse drug reaction (ADR) is a harmful response to a drug at normal doses-like a rash or liver damage. An adverse drug event (ADE) is broader: it includes ADRs, but also medication errors, overdoses, and interactions. So all ADRs are ADEs, but not all ADEs are ADRs.
Can I prevent ADEs on my own?
Yes. Keeping a full list of your medications, asking questions at every appointment, and checking with your pharmacist about interactions are three of the most effective ways to prevent harm. You don’t need to be a medical expert-you just need to be informed and proactive.
Which medications are most likely to cause ADEs?
The top three are anticoagulants (like warfarin), diabetes drugs (especially insulin), and opioids. These drugs have narrow safety margins, meaning small mistakes can lead to serious harm. Warfarin alone causes over 33,000 emergency visits each year in the U.S.
Are herbal supplements safe to take with prescription drugs?
No-many are not. St. John’s Wort can make birth control, antidepressants, and blood thinners less effective. Garlic and ginkgo can increase bleeding risk with warfarin. Turmeric can interfere with blood sugar control. Always tell your doctor and pharmacist about every supplement you take.
How do I know if my pharmacist is helping me prevent ADEs?
Ask if they offer Medication Therapy Management (MTM). This is a free service where a pharmacist reviews all your medications, checks for interactions, and helps you understand what you’re taking. If they’re not offering it, ask why. You deserve this level of care.
Is it safe to stop a medication if I think it’s causing side effects?
Never stop a medication without talking to your doctor first. Some drugs, like blood pressure pills or antidepressants, can cause dangerous withdrawal symptoms if stopped suddenly. Instead, write down your symptoms and bring them to your next appointment. Your doctor can help you decide if it’s safe to adjust or stop the drug.
Karl Barrett
December 2, 2025 AT 07:00
Let’s be real-ADEs aren’t just clinical failures, they’re systemic ones. We’ve got this insane pharmacopeia of drugs that work great in RCTs but collapse under real-world polypharmacy. The real kicker? We treat meds like candy. You get a script, you take it, no questions. But the pharmacokinetics of a 72-year-old on 8 meds ain’t the same as a 30-year-old in a trial. We need to stop outsourcing safety to algorithms and start treating patients as complex, dynamic systems. Genomics, AI, MTM-they’re tools, not magic wands. The human layer is still the bottleneck.
Jake Deeds
December 3, 2025 AT 13:18
Wow. Just wow. I mean, I knew meds were dangerous, but I didn’t realize we were basically playing Russian roulette with insulin and warfarin. Like, who let this happen? Someone’s gotta pay for this. It’s not just negligence-it’s institutional arrogance. People die because doctors are too busy scrolling through their phones to check for interactions. And don’t even get me started on pharmacies that still use paper scripts. We’re in 2024. This is medieval.
Isabelle Bujold
December 5, 2025 AT 01:30
As a pharmacist in Ontario, I see this every day. The most preventable ADEs? Those involving seniors on anticoagulants who don’t understand INR targets, or those who’re taking OTC NSAIDs on top of their warfarin because ‘it’s just ibuprofen.’ The biggest gap isn’t tech-it’s education. We have MTM services available for free through provincial plans, yet only 12% of eligible patients use them. Most think it’s just a pill count. It’s not. It’s a 45-minute deep dive into their entire regimen, including ginkgo, turmeric, and that ‘natural’ sleep aid from the health food store. We need to rebrand MTM as ‘medication wellness coaching.’ Make it feel less clinical, more like a conversation with someone who actually cares.
michael booth
December 5, 2025 AT 17:16
I work in a hospital pharmacy and can confirm every single point here. The numbers don't lie. The most effective intervention we've seen? Medication reconciliation at discharge. It's simple, it's free, and it saves lives. We've cut our 30-day readmission rate by 31% just by doing it right. But it takes time. And time is the one thing nobody has. Still. Worth it.
Shofner Lehto
December 7, 2025 AT 01:51
My mom had a near-fatal ADE from a drug interaction she never knew about. She took St. John’s Wort for ‘mild anxiety’ and didn’t think it counted as a drug. She didn’t tell her doctor. The pharmacist didn’t ask. The system failed her. Now I carry a laminated list of her meds in my wallet. I’ve made my whole family do the same. You don’t need an MD to be your own advocate. Just a pen, a notebook, and the guts to ask ‘why?’
Yasmine Hajar
December 7, 2025 AT 07:00
Let’s talk about the elephant in the room: profit. Pharma spends billions marketing drugs but next to nothing on patient safety education. Why? Because a patient who knows how to prevent an ADE is a patient who doesn’t need more pills. The system is designed to keep you on meds, not to get you off them. Deprescribing is the radical act here. It’s not just medical-it’s political. If you’re over 65 and on more than 5 meds, you’re not being cared for. You’re being monetized. And if you’re not angry about that, you should be.
val kendra
December 7, 2025 AT 21:04
Biggest thing I learned working ER? People don’t know how to read their own prescriptions. I had a guy come in with a sugar crash because he thought ‘10 units’ meant 10 pills. He had insulin pens. He didn’t know how to use them. No one ever showed him. No one ever asked if he understood. We’re treating complex chronic conditions like they’re a grocery list. We need to stop assuming literacy. And start assuming ignorance-and then educate. Like, really educate. Not hand them a pamphlet and say ‘call if you have questions.’
John Filby
December 8, 2025 AT 05:20
Just got my first MTM session yesterday. Pharmacist sat with me for 40 mins, found 3 meds I didn’t need, caught a bad interaction between my blood pressure pill and my fish oil, and even helped me switch to a cheaper generic. I didn’t even know this was free. Why isn’t this advertised everywhere? Like on TV? On your prescription bottle? This is the most valuable health service most people don’t know exists.
Elizabeth Crutchfield
December 8, 2025 AT 16:00
i never knew the diff between ade and adr til now. wow. my grandpa died from a bad interaction and no one ever told us it coulda been prevented. thanks for this.