Generic Drug Approval: What You Need to Know About Safety, Equivalence, and Real-World Use
When you hear generic drug approval, the process by which regulatory agencies like the FDA verify that a generic version of a brand-name drug is safe, effective, and interchangeable. Also known as therapeutic equivalence certification, it's not just about matching ingredients—it's about making sure your body reacts the same way. Many people assume all generics are created equal, but the truth is more complex. The FDA doesn’t just check if the active ingredient is the same. They require the generic to deliver the same amount of medicine into your bloodstream at the same speed as the brand name. That’s bioequivalence. If it’s off by more than 5%, it gets rejected. No exceptions.
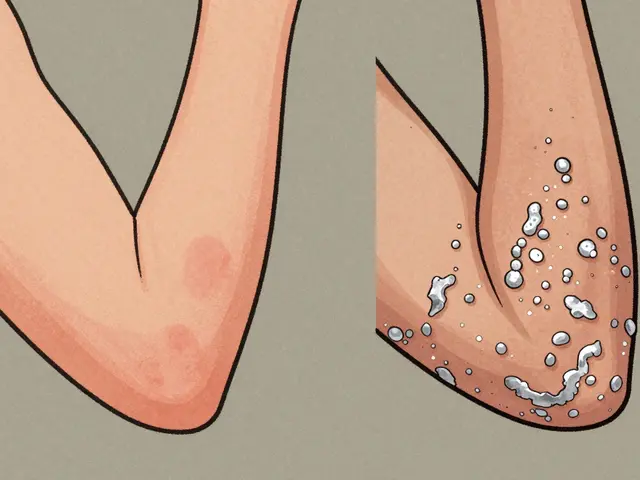
This process matters because generic medications, lower-cost versions of brand-name drugs that must meet the same strict standards as their branded counterparts. Also known as generic equivalents, they make up over 90% of prescriptions in the U.S. But not all generics perform the same in real life. Providers report cases where switching from one generic to another—even both FDA-approved—caused unexpected side effects or loss of control in conditions like epilepsy or thyroid disease. Why? Because inactive ingredients (fillers, dyes, coatings) can affect how the drug dissolves. One pill might release too fast. Another too slow. And for drugs with narrow therapeutic windows—like warfarin, lithium, or levothyroxine—that tiny difference can mean the difference between safety and danger.
Therapeutic equivalence, the official FDA rating that tells you a generic can be substituted for a brand-name drug without changing clinical outcomes. Also known as AB rating, it’s your best guide when choosing between options. Drugs rated AB are considered interchangeable. But not every generic gets that rating. Some are listed as BX, meaning there’s not enough data to confirm they’re fully equivalent. And here’s the catch: the FDA doesn’t test every batch of every generic every time. They rely on manufacturer data, inspections, and post-market reports. That’s why FDA approval, the formal authorization granted by the U.S. Food and Drug Administration allowing a drug to be sold in the U.S. market. Also known as NDA or ANDA approval, it’s the starting point—not the finish line. Real-world safety depends on ongoing monitoring through systems like FAERS, where patients and doctors report unexpected reactions. That’s how we learn that a generic made by one company works great for most, but causes nausea or headaches in others.
And then there’s the brand vs generic, the comparison between name-brand pharmaceuticals and their lower-cost, chemically identical alternatives. Also known as originator vs generic, this debate isn’t just about price—it’s about trust. Some people swear by their brand. Others save hundreds a month with generics and feel no difference. The truth? For most drugs, generics work just as well. But for a small group—people on critical meds, with complex conditions, or who’ve had bad experiences—it’s not a gamble they’re willing to take. That’s why provider case studies show real variation: one doctor sees no issues. Another sees patients crashing after a switch. It’s not about quality control failures. It’s about biological variability and how your body responds to tiny differences in formulation.
What you’ll find below isn’t just theory. It’s real stories from doctors, patients, and pharmacists who’ve seen what happens when generics are switched too quickly, bought from shady online sources, or assumed to be perfect copies. You’ll learn how to spot red flags, when to push back on a substitution, and how to use FDA databases to check if your drug has a history of problems. This isn’t about fear. It’s about knowing what to ask, when to speak up, and how to make sure your treatment stays safe—even when the label says it’s just a generic.