Adverse Event Database: What It Is and Why It Matters for Your Medication Safety
When a medicine causes unexpected harm, it doesn’t just disappear into thin air—it gets recorded in an adverse event database, a centralized system that collects and analyzes reports of harmful reactions to medications. Also known as pharmacovigilance databases, these systems are the backbone of drug safety monitoring worldwide. Think of them as early warning networks. Every time someone reports a strange side effect—like sudden dizziness after starting a new pill, or unexplained bruising while on blood thinners—that data flows into these databases. They don’t just store reports; they connect the dots between drugs, symptoms, and patient profiles to spot hidden dangers before they hurt more people.
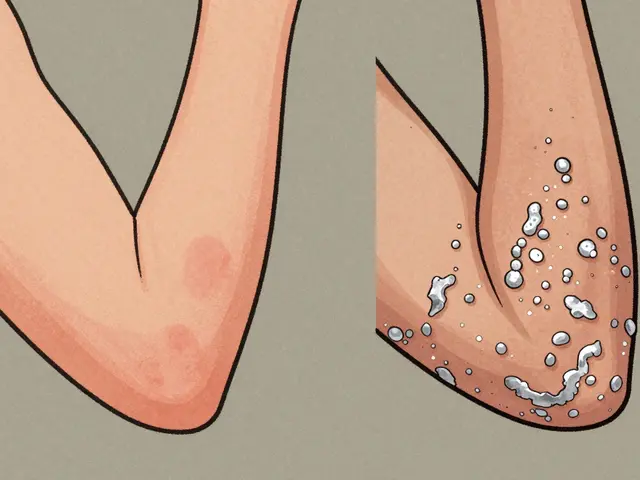
These databases rely on inputs from real people: patients, doctors, pharmacists, and even manufacturers. The adverse drug reactions, harmful and unintended responses to a drug at normal doses recorded here aren’t just minor nuisances. They include liver damage from statins, dangerous bleeding from warfarin interactions with alcohol, or sudden drops in clozapine levels when someone quits smoking. These aren’t theoretical risks—they’re documented events that led to label changes, dosage warnings, or even drug withdrawals. And it’s not just about prescription drugs. Herbal supplements, over-the-counter painkillers, and even counterfeit pills laced with fentanyl show up in these systems too. The medication safety, the practice of preventing harm caused by medicines you get from your pharmacist isn’t magic—it’s built on years of data collected in these databases.
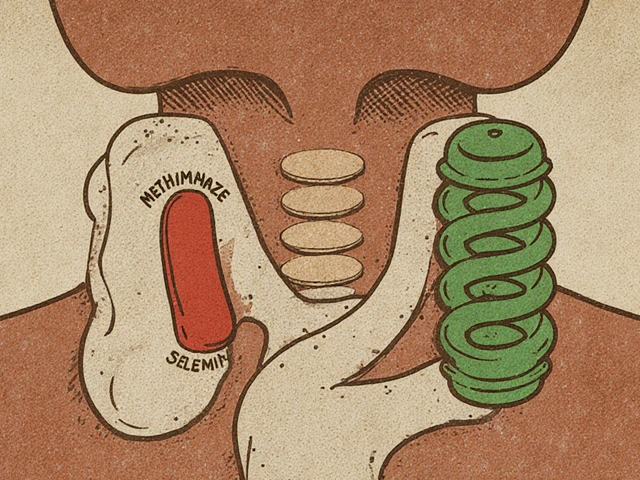
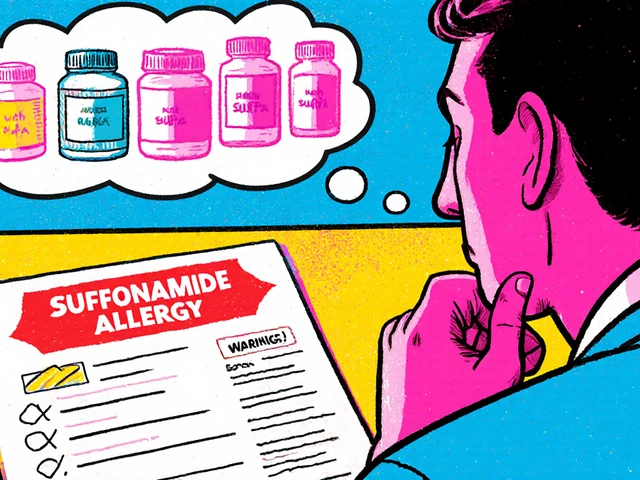
What makes these systems powerful is how they turn isolated incidents into patterns. One person’s nausea might be ignored. But when hundreds report the same issue after taking a generic version of a drug, regulators take notice. That’s how safety alerts get issued. That’s how doctors learn to avoid dangerous combinations, like mixing certain antivirals with statins that affect liver enzymes. And that’s why your report matters—even if you think it’s "just a side effect." If enough people report it, it becomes part of the evidence that protects the next patient.
Below, you’ll find real stories and studies from people who’ve dealt with these issues firsthand—from providers who’ve seen dangerous generic substitutions to patients who learned the hard way how alcohol changes their INR levels. These aren’t abstract concepts. They’re the raw material that feeds the adverse event database. And understanding how it works helps you ask better questions, spot red flags, and stay safer.