Provider Experiences: Real Insights on Medication Safety and Patient Care
When healthcare providers talk about provider experiences, the real-world observations and decisions clinicians make while managing medications and patient responses. Also known as clinical practice insights, it’s not just about following guidelines—it’s about noticing what happens when pills meet real lives. These aren’t textbook cases. They’re the stories behind the data: the patient who stopped taking clozapine after quitting smoking and ended up in the ER, the person who split their pill to save money and got sick because the tablet wasn’t designed for it, the nurse who caught a fake fentanyl pill because the imprint looked off. Provider experiences are where theory meets the messy reality of human bodies, habits, and systems.
These experiences tie directly to medication safety, the practice of preventing harm caused by drugs through proper use, monitoring, and communication. A single misread label, a missed interaction between protein shakes and levothyroxine, or not knowing that sulfonamide allergies don’t always mean avoiding all sulfa drugs can change a patient’s outcome. Providers see this daily. They notice when a patient’s TSH spikes because they drank a protein shake right after taking their thyroid pill. They catch when someone’s statin is raising blood sugar—not because the drug is broken, but because the wrong one was chosen for their metabolic profile. And they’re the ones who know that adverse drug reactions, harmful, unintended responses to medications that go beyond expected side effects aren’t always the drug’s fault. Sometimes, they’re triggered by fear, misinformation, or the nocebo effect—where expecting side effects makes them happen.
Then there’s drug interactions, how one medication changes how another works in the body, often through liver enzymes like CYP1A2 or P-glycoprotein. Providers track these like chess moves. Smoking cuts clozapine levels in half. Grapefruit juice can turn a safe dose of a statin into a toxic one. Even something as simple as timing your antiviral with a meal can make or break treatment. These aren’t theoretical risks—they’re daily decisions that shape prescriptions. And behind every interaction is a patient who didn’t know, or couldn’t afford, the right advice.
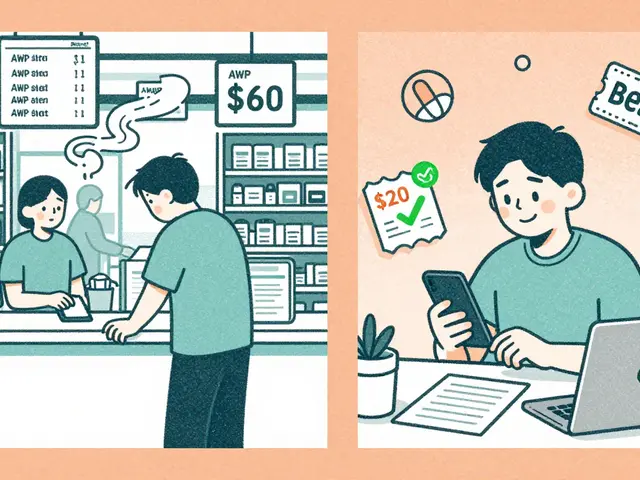
What ties it all together is patient-centered care, an approach that puts the individual’s needs, values, and lived experience at the heart of medical decisions. It’s not just about giving the right drug. It’s about asking: Can you afford this? Do you understand the label? Are you scared of side effects because of what you read online? Are you hiding your smoking habit because you think it’ll get you judged? Providers who listen—really listen—catch the gaps that checklists miss. They help patients split pills safely, find legal ways to buy generics, or recognize fake pills before it’s too late.
What you’ll find in this collection isn’t theory. It’s the kind of practical, hard-won knowledge that comes from clinics, pharmacies, and patient rooms. You’ll see how real providers navigate complex drug interactions, spot dangerous side effects, and help people make smarter choices without judgment. Whether you’re a patient trying to understand your meds or a provider looking for clearer guidance, these stories and guides are built on what actually works—and what almost didn’t.