Chronic Kidney Disease (CKD) – Overview & Resources
When dealing with Chronic Kidney Disease, a progressive loss of kidney function that impairs waste removal, fluid balance, and hormone regulation. Also known as CKD, it affects millions worldwide and touches many other health topics. For instance, secondary hyperparathyroidism, excess parathyroid hormone production caused by low kidney function often develops as kidneys fail to keep calcium and phosphate in check. Managing fluid overload usually means turning to diuretics, medications that increase urine output to control fluid and blood pressure. And because CKD patients are at higher risk for clotting problems, careful use of blood thinners, anticoagulant drugs that prevent harmful clots becomes a daily concern. These connections form the backbone of what you’ll see in the articles below.
How CKD Shapes Treatment Choices
One clear semantic link is that chronic kidney disease encompasses secondary hyperparathyroidism; the dropping glomerular filtration rate triggers hormonal imbalances that strain the bones and cardiovascular system. That imbalance often leads doctors to consider parathyroidectomy, a surgical option that removes overactive parathyroid glands. The decision hinges on how severe the hormone excess is and whether medical therapy can control it. Meanwhile, diuretics play a dual role: they lower blood pressure—a key factor that slows CKD progression—and they help manage edema, a common symptom when kidneys can’t excrete excess fluid.
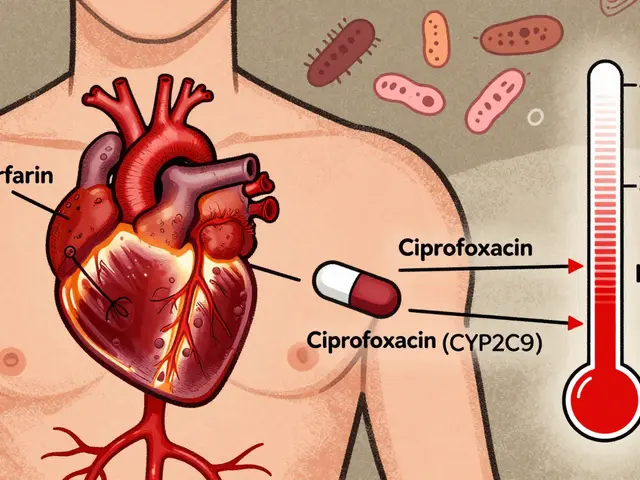
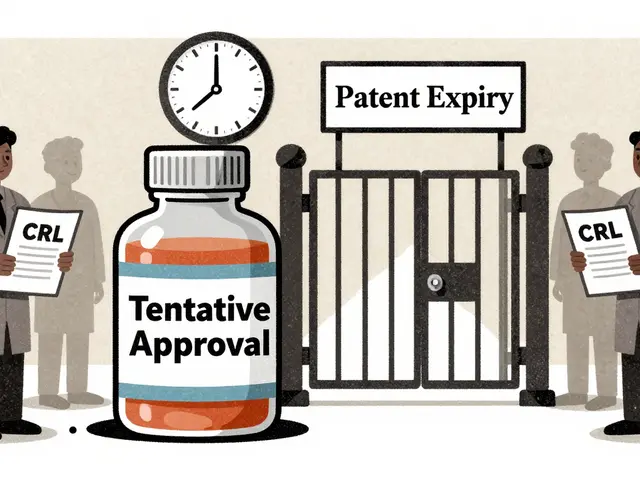
Blood thinners add another layer of complexity. Warfarin, for example, has been a staple for decades, but newer direct oral anticoagulants (DOACs) offer easier monitoring and fewer dietary restrictions. However, DOACs are cleared partially through the kidneys, so dosing must be adjusted for CKD stages. This relationship—CKD requires careful anticoagulant management—shows why patients often switch between warfarin and DOACs based on kidney function trends.
Dietary considerations also tie into these medical choices. Sodium restriction helps diuretics work better, while limiting phosphate intake curbs secondary hyperparathyroidism. Vitamin D supplements may be needed, but renal conversion is impaired, so active forms like calcitriol become necessary. All these pieces—hormone control, fluid balance, clot prevention, and nutrition—interlock to form a comprehensive CKD care plan.
In practice, clinicians use a step‑by‑step algorithm: first assess kidney function, then screen for calcium‑phosphate disturbances, decide if diuretics or blood thinners are appropriate, and finally evaluate whether surgical intervention like parathyroidectomy is justified. Each step reflects a semantic triple: CKD influences secondary hyperparathyroidism; secondary hyperparathyroidism guides parathyroidectomy decisions; and CKD dictates blood thinner dosing.
Below you’ll find a curated set of articles that dig deeper into each of these topics. Whether you’re looking for a practical buying guide for medications, a side‑by‑side drug comparison, or a surgical overview, the collection offers clear, actionable information to help you navigate chronic kidney disease management effectively.