Cholesterol meds save lives, but they're not one-size-fits-all.
If you're trying to lower LDL, know the main options and how they differ.
Statins are the most common choice. Drugs like atorvastatin, simvastatin, and rosuvastatin reduce LDL by blocking cholesterol production in your liver. They cut heart attack risk for many people. Side effects can include muscle aches, mild liver enzyme changes, and rarely more serious muscle injury. If statins cause problems, doctors may switch doses or try a different statin.
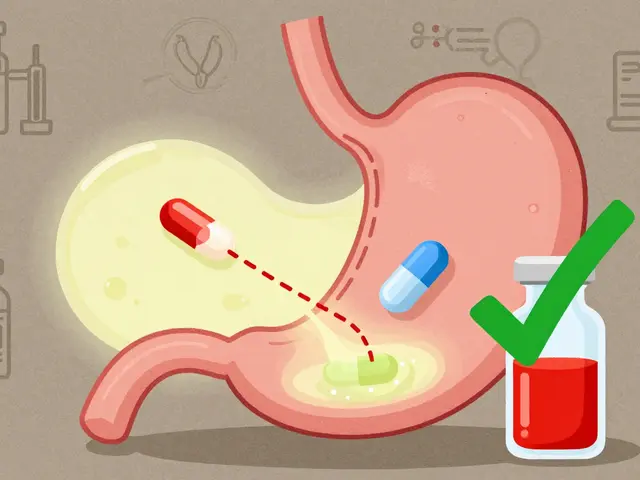
Ezetimibe works differently. It lowers LDL by reducing cholesterol absorption in the gut. Often combined with a statin (Vytorin is simvastatin plus ezetimibe), ezetimibe gives an extra LDL drop without adding many side effects. It’s a good option when statins alone don’t reach targets.
PCSK9 inhibitors are injectable drugs for people with very high LDL or those who don’t tolerate statins. These newer meds, such as evolocumab and alirocumab, can dramatically cut LDL by 50% or more. They’re expensive and usually prescribed after other options fail, but they help people at high risk.
Inclisiran is a newer twice-yearly injection that uses RNA interference to lower LDL. It’s convenient and effective, and may suit people who struggle with daily pills. Long-term outcome data is building, but early results are promising.
Fibrates and niacin target triglycerides and can help specific conditions. Fibrates work well when triglycerides are the main issue. Niacin raises HDL but has fallen out of favor because outcome benefits are unclear and side effects can be bothersome.
Bile acid sequestrants like colesevelam bind bile in the gut and lower LDL. They can cause constipation and interfere with absorption of other drugs, so timing and monitoring matter.
If you’re statin-intolerant, alternatives include lower-dose statin plus ezetimibe, PCSK9 inhibitors, inclisiran, or lifestyle-first strategies. Some people try plant sterols, soluble fiber, and omega-3s; these help modestly and are safe with drugs.
How to pick the right one? Think risk first. Your 10-year cardiovascular risk, personal history, and LDL level guide choices. If you’ve had a heart attack, more aggressive lowering is usually better. If your risk is low, lifestyle changes may be enough.
Watch for interactions. Common meds, grapefruit juice, and some supplements affect statin levels. Tell your doctor about everything you take. Always check liver tests and ask about muscle pain.
Practical tips: keep a list of your meds, refill before you run out, and get copy of your lipid results. If you shop online for meds, use licensed pharmacies, require prescriptions, and avoid unusually low prices that seem too good to be true.
Questions to ask your doctor: What LDL target should I aim for? What are the realistic benefits and risks for me? Can we try a lower dose or an alternative if I get side effects?
If you’re unsure, get a second opinion or pharmacist advice; small changes compound over months, so track results and celebrate progress with your care team regularly.