Brand vs Generic Medications: What You Really Need to Know
When you see a prescription for brand vs generic, the difference between name-brand drugs and their lower-cost copies. Also known as name-brand drugs, it’s not about quality—it’s about patents, pricing, and sometimes, misinformation. Most people assume generics are weaker or made with cheaper ingredients. That’s not true. The FDA requires generic drugs to have the same active ingredient, strength, dosage form, and route of administration as the brand name. They must also work the same way in your body. If your doctor prescribes Lipitor and you get atorvastatin instead, you’re getting the exact same medicine—just without the fancy packaging or marketing budget.
So why do brand names cost so much more? It’s simple: drug companies spend millions developing a new drug, running clinical trials, and getting approval. Once the patent runs out, other manufacturers can make the same drug. They don’t have those upfront costs, so they sell it for a fraction of the price. That’s how generic medication, lower-cost versions of brand-name drugs approved by regulatory agencies. Also known as generic drugs, it becomes a smart choice for millions. But here’s the catch: not all generics are made the same. Some are produced in facilities with poor quality control. That’s why buying from licensed pharmacies matters. You wouldn’t risk your health with fake pills—same goes for unverified online sellers offering ultra-cheap generics. The posts below show real cases where people saved hundreds on medication costs, the total expense of prescription drugs over time. Also known as drug expenses, it by switching to generics—without losing effectiveness.
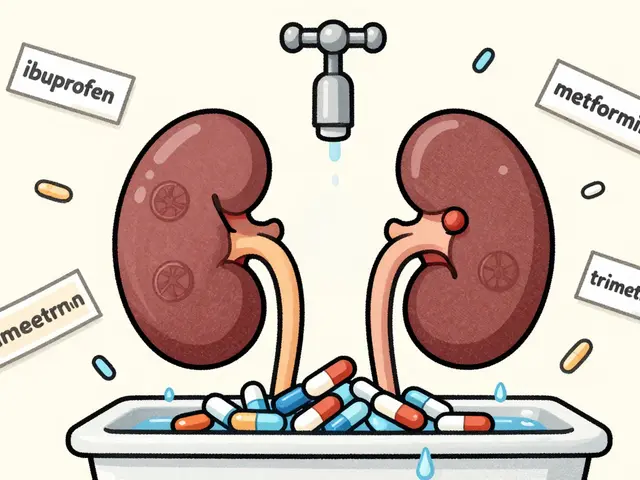
But it’s not always straightforward. Some drugs, like warfarin or levothyroxine, need very precise dosing. Even tiny differences in inactive ingredients can affect how your body absorbs them. That’s why some doctors stick with brand names for these. Others, like clozapine or praziquantel, have complex interactions with food, smoking, or other meds—so switching brands can change how well they work. The posts here cover exactly these situations: when switching saves money, and when it could backfire. You’ll find real stories about people splitting pills, buying online, and choosing between generics and brands—and what actually happened.
There’s also the psychological side. If you’ve been on a brand-name drug for years, your body might feel more familiar with it—even if it’s chemically identical. That’s not placebo; it’s real. Your brain trusts the name you’ve seen for decades. But that doesn’t mean the generic won’t work. It just means you might need to give it time. And if you notice changes—like new side effects or less control over your condition—talk to your pharmacist. They can help you figure out if it’s the drug, the filler, or something else.
Bottom line: brand vs generic isn’t about which is better. It’s about which is right for you. For most people, generics are safe, effective, and save money. For others, sticking with the brand makes sense. The key is knowing when to switch, when to ask questions, and where to buy safely. Below, you’ll find real, practical guides on how to do exactly that—without falling for scams, saving money the right way, and understanding exactly what’s in your pills.