Alcohol and Warfarin: What You Need to Know About the Dangerous Mix
When you take warfarin, a blood thinner used to prevent dangerous clots in people with atrial fibrillation, deep vein thrombosis, or artificial heart valves. Also known as Coumadin, it works by blocking vitamin K, which your body needs to make clotting factors. But if you drink alcohol, a substance that affects liver enzymes responsible for breaking down warfarin, things get risky fast. Even a single drink can throw off your INR levels — the test that measures how long it takes your blood to clot. Too high, and you risk bleeding inside your brain, stomach, or joints. Too low, and you could get a stroke or pulmonary embolism.
It’s not just about how much you drink — it’s about consistency. If you usually have one glass of wine with dinner and suddenly skip it for a week, your warfarin dose might become too strong. If you binge drink on the weekend, your liver slows down warfarin metabolism, making it build up in your system. Both scenarios are dangerous. Studies show that heavy drinkers on warfarin have up to a 30% higher chance of major bleeding. And it’s not just beer or wine — spirits, cocktails, and even some cough syrups with alcohol can do the same thing. Your doctor doesn’t need to know you had a party last night — they need to know your drinking pattern so they can adjust your dose properly.
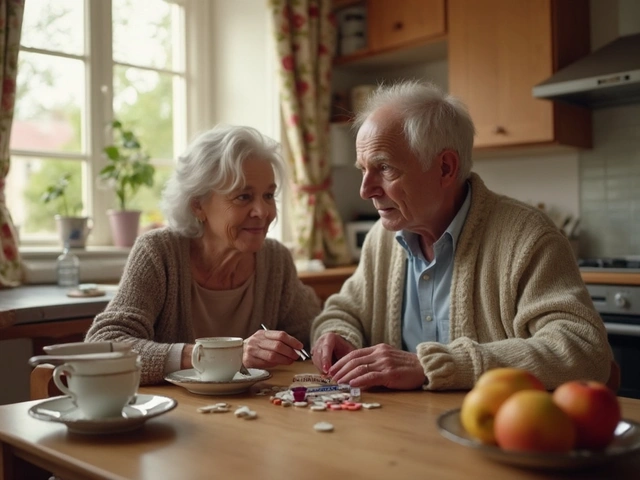
Some people think they can just avoid alcohol completely to stay safe. But that’s not always the answer either. For many, a small, regular amount — like one drink a day — is actually safer than going cold turkey. The key is stability. If you’ve been drinking moderately for months, keep doing it. If you don’t drink, don’t start. Don’t try to "catch up" after a dry week. Don’t drink to relieve stress while on warfarin — that’s when mistakes happen. The real enemy isn’t alcohol itself — it’s inconsistency.
And don’t forget about other things that interact with warfarin. vitamin K, found in leafy greens like spinach and kale, can weaken warfarin’s effect. If you suddenly start eating a lot more kale, your INR will drop. Same goes for certain antibiotics, like metronidazole or ciprofloxacin — they can spike your INR without warning. That’s why regular blood tests aren’t optional. They’re your lifeline.
There’s no magic number for "safe" alcohol on warfarin — it depends on your liver, your dose, your diet, and your habits. But here’s what every patient needs to know: if you drink, tell your doctor. If you change how much you drink, get your INR checked. If you feel dizzy, bruise easily, or notice blood in your urine or stool — stop drinking and call your doctor right away. This isn’t about fear. It’s about control. You’re not giving up life — you’re learning how to live safely with a powerful medicine. And the posts below show real cases, expert advice, and practical tips from people who’ve been there — from managing INR spikes after a holiday party to knowing when to skip the beer entirely.