When you fill a prescription for a medication like Protonix or Ocella, you might not realize you're getting something called an authorized generic. It looks different from the brand-name pill, has no brand name on the label, and costs significantly less-but it’s exactly the same drug, made by the same company, in the same factory. For insurance companies, this isn’t just a cheaper option. It’s a strategic tool to lower costs without risking patient outcomes. But how do insurers decide where to put these drugs in their formularies? And why does it matter to you?
What Exactly Is an Authorized Generic?
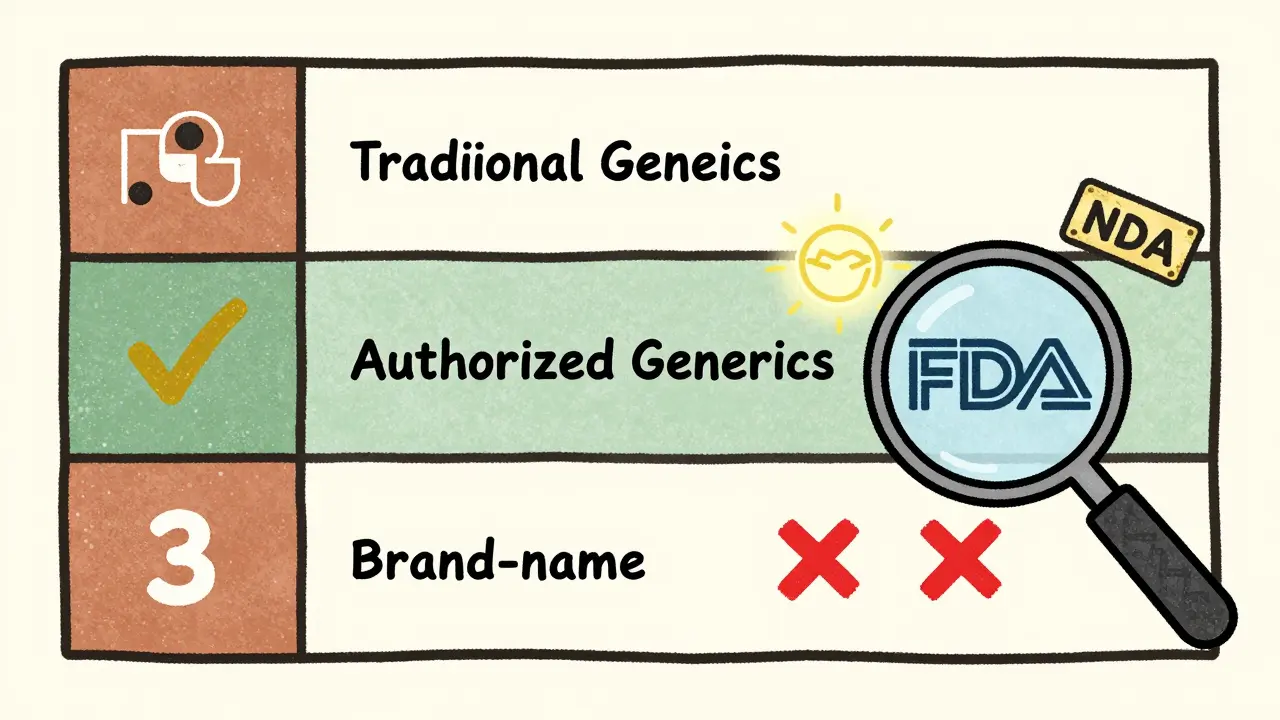
An authorized generic isn’t a knockoff. It’s not a generic made by a different company trying to copy the brand. It’s the exact same medication as the brand-name version, produced under the original manufacturer’s New Drug Application (NDA). The FDA defines it as a drug approved under an NDA that’s sold under different packaging or labeling, but with identical active and inactive ingredients. Think of it like buying a car from the same factory but without the logo on the hood.
Unlike traditional generics-which must prove they’re bioequivalent through lengthy ANDA applications-authorized generics skip that step entirely. They’re already approved. That means they hit the market faster, often right when the brand patent expires. No waiting. No delays. And because they’re made by the brand manufacturer, there’s zero risk of differences in how the drug works in your body.
As of 2023, the FDA lists 147 authorized generics. Common ones include Synthroid, Yasmin, and Protonix. These aren’t niche products. They’re widely prescribed drugs for conditions like thyroid disorders, birth control, and acid reflux. The key difference? You pay generic prices for a brand-quality product.
Why Insurers Care About Formulary Placement
Insurance plans organize drugs into tiers. Tier 1 is usually the cheapest-often traditional generics. Tier 2 and 3 are higher-cost drugs, sometimes including brand-name medications. The goal? Encourage patients to pick lower-cost options without sacrificing effectiveness.
Authorized generics fit perfectly into Tier 2. Why? Because they’re therapeutically identical to the brand, but cost 15-25% less. That’s huge for insurers. A 2022 study of 1,247 Medicare Part D plans found that 87% of them placed authorized generics in the same tier as traditional generics. Only 12% treated them like brand-name drugs. That means lower copays for patients and lower overall spending for the plan.
For example, if your brand-name Synthroid costs $50 per prescription with a $40 copay, the authorized generic might cost $30 with a $10 copay. That’s not just savings-it’s predictability. No need to switch medications, no risk of allergic reactions to new inactive ingredients, and no confusion about whether the drug will work the same way.
How Authorized Generics Compare to Traditional Generics
Many people assume all generics are the same. They’re not. Traditional generics are made by third-party manufacturers who must prove bioequivalence. Authorized generics are made by the original brand manufacturer-same formula, same equipment, same quality control.
Here’s how they stack up:
| Feature | Authorized Generic | Traditional Generic |
|---|---|---|
| Manufacturer | Original brand company | Third-party generic maker |
| Approval Path | Under original NDA | Abbreviated New Drug Application (ANDA) |
| Bioequivalence Testing | Not required | Required |
| Time to Market | Immediately after patent expires | After ANDA approval (often delayed) |
| Formulary Tier | Usually Tier 2 (same as traditional generics) | Usually Tier 1 or 2 |
| Availability | Only 15-20% of brand drugs have them | Available for most drugs |
The biggest advantage? No therapeutic substitution risk. If you’re on a drug with a narrow therapeutic index-like warfarin or levothyroxine-even tiny differences in how the drug is absorbed can cause problems. Authorized generics eliminate that risk entirely.
Real Patient Experiences
On Reddit’s r/Pharmacy community, users shared stories about how authorized generics changed their lives. One person wrote: "My insurance denied Synthroid because it was branded. The authorized generic? Approved with a $10 copay. My TSH levels stayed perfect. No issues." Another said they switched after developing a rash from a traditional generic-only to find the authorized version didn’t trigger the reaction because the inactive ingredients matched the brand.
But it’s not always smooth. A 2022 GoodRx survey found that 34% of patients didn’t know they were getting an authorized generic until they saw the pill look different. Some got denied coverage because their pharmacy’s system didn’t recognize the NDC code. One woman spent three weeks fighting her insurer after her prescription switched without notice. She ended up paying $80 out of pocket before the claim was corrected.
Pharmacy benefit managers (PBMs) are improving. Express Scripts reported 89% of authorized generic claims were approved on the first try in 2023-close to the 92% approval rate for traditional generics. But that still leaves 11% of claims that need manual review. That’s time, frustration, and sometimes delays in treatment.
How Insurers Actually Implement Coverage
Putting authorized generics on a formulary isn’t as simple as adding a new drug. It requires updating pharmacy systems, training staff, and coding the correct NDC numbers. Many systems still treat them like brand-name drugs because they’re not listed in the FDA’s Orange Book (which only includes traditional generics).
CVS Caremark says it takes 30-45 days from product launch to full system integration. Walgreens reported a 12% error rate in early processing before they added special verification steps. Prime Therapeutics’ AG Tracker database now covers 98% of available authorized generics, helping insurers stay ahead.
The key? Insurers need to know which products are authorized generics. The FDA publishes a public list. PBMs use proprietary tools. Pharmacists need training. Prescribers need to know to write "authorized generic" on the script if they want to ensure coverage.

Market Trends and Regulatory Shifts
The U.S. authorized generic market hit $4.7 billion in 2022. That’s 3.2% of the total generic drug market-but growing fast. Analysts project an 8.4% annual growth rate through 2027. Why? Because it’s a win-win for manufacturers and payers.
Brand manufacturers use authorized generics to keep market share after patent expiry. Instead of losing everything to competitors, they keep selling under a different label. It’s legal, it’s smart, and it’s profitable.
But there’s a catch. The FTC found in 2022 that authorized generics delayed true generic competition in 22% of cases. If the brand manufacturer launches its own generic right away, other companies might not bother entering the market. That’s why regulators are watching closely.
Meanwhile, the Inflation Reduction Act is pushing Medicare Part D to favor lower-cost options. By 2025, CMS expects a 15-20% increase in authorized generic usage. Large employers are already planning to differentiate coverage: 68% of them intend to offer better copays for authorized generics over traditional ones in 2024.
What This Means for You
If you’re on a long-term medication, ask your pharmacist: "Is there an authorized generic for this?" If there is, and your insurance covers it, you could save hundreds a year. Don’t assume the generic you’re getting is the cheapest option.
Check your formulary. Look for drugs with "authorized generic" listed. If it’s not there, ask your insurer why. Some plans still treat them like brand drugs. That’s outdated. With FDA approval and identical chemistry, they belong in the lowest cost tier.
And if you’ve ever had a reaction to a generic? The authorized version might be your solution. Same drug. Same ingredients. Just cheaper.
Are authorized generics as safe as brand-name drugs?
Yes. Authorized generics are made by the same manufacturer, in the same facility, with the exact same active and inactive ingredients as the brand-name drug. The FDA considers them therapeutically equivalent. There is no increased risk of side effects or reduced effectiveness.
Why don’t all drugs have authorized generics?
Only about 15-20% of brand-name drugs have authorized generic versions. This happens when the original manufacturer decides to produce and market its own generic version after patent expiration. Many companies choose not to, either because they want to exit the market or because they’re waiting for other generics to enter. It’s a business decision, not a regulatory one.
Can my pharmacy switch me to an authorized generic without telling me?
Yes, unless your prescription specifically says "do not substitute." Pharmacists are allowed to substitute authorized generics just like traditional generics. But many patients don’t notice the change because the pill looks different or the packaging is unfamiliar. Always check your medication when you pick it up.
Do Medicare Part D plans cover authorized generics?
Yes. Since 2021, CMS has confirmed that authorized generics qualify for the same coverage as traditional generics under Medicare Part D. They must be placed in the same formulary tier and charged the same copayment. If your plan denies coverage, ask them to check the FDA’s list and update their system.
How do I find out if my drug has an authorized generic?
Visit the FDA’s official list of authorized generic drugs at fda.gov/drugs/informationondrugs/authorizedgenerics. You can search by brand name. Your pharmacist can also check using proprietary databases like Prime Therapeutics’ AG Tracker. If your drug isn’t listed, it likely doesn’t have one.
Next Steps for Patients and Providers
If you’re a patient: Ask your pharmacist or doctor if an authorized generic exists for your medication. If it does, ask your insurer to confirm coverage. If you’re denied, request a review-your drug should be covered at the generic tier.
If you’re a prescriber: When writing prescriptions, consider specifying "authorized generic" if available. This reduces confusion and ensures the right drug is dispensed. Update your formulary guides to include authorized generics as equivalent to brand-name drugs.
If you’re part of a health plan: Review your formulary. Move authorized generics into the lowest cost tier. Train your pharmacy network. Update your systems. The savings are real, the safety is proven, and the patient experience is better.

Sam Dickison
February 8, 2026 AT 08:11
Authorized generics are a stealth win for payers and patients alike. You get the exact same drug, same factory, same QA - just without the brand markup. Insurers should be pushing these to Tier 1, not Tier 2. The FDA’s NDA-based approval means zero bioequivalence uncertainty. Why are we still treating them like second-class generics? This isn’t about cost-cutting - it’s about rational formulary design.
And let’s be real: if your PBM can’t differentiate between an authorized generic and a brand, that’s a system failure, not a patient issue.
Karianne Jackson
February 9, 2026 AT 13:51
I got switched to an authorized generic and thought I was getting scammed. The pill looked totally different. I almost called the cops.
Tom Forwood
February 10, 2026 AT 15:55
Yo, I’ve been on Synthroid for 8 years. Switched to the authorized generic last year and my TSH? Still perfect. No drama. No weird side effects. Just cheaper.
My pharmacist didn’t even tell me until I asked why the bottle looked different. Honestly? I was kinda mad at first. Then I saw the $12 copay vs $48. Now I’m like - why isn’t everyone doing this?
Also, if you’ve had a rash from a generic? Try the authorized one. Same active ingredient, different filler. Could be the fix. Just sayin’.
Jacob den Hollander
February 12, 2026 AT 04:53
Wow. I didn’t realize how much this mattered until my mom got switched to an authorized generic for her blood pressure med. She was terrified - thought they were giving her ‘fake’ medicine. I had to sit down with her, show her the FDA page, explain the NDA thing...
Turns out, she’d been getting a traditional generic for years that made her dizzy. The authorized one? Zero issues. She’s now a convert.
Pharmacists need to do better. This isn’t just a cost thing - it’s a trust thing. People need to know they’re not being swapped out for something sketchy. And insurers? Stop treating these like they’re ‘lesser.’ They’re not.
Also, if your script says ‘do not substitute,’ that’s your right. Use it. And if your pharmacy ignores it? File a complaint. Seriously.
Biggest takeaway? Authorized generics = brand quality. No compromises. Just savings. Why isn’t this on every pharmacy counter?
Andrew Jackson
February 13, 2026 AT 13:00
It is a fundamental dereliction of duty by the FDA to permit pharmaceutical manufacturers to exploit regulatory loopholes under the guise of consumer savings. The authorized generic model is a cynical maneuver designed to preserve monopolistic pricing structures under the veneer of competition. It is not innovation - it is market manipulation. The FTC’s findings are not incidental; they are damning. This is corporate capture of public health policy at its most insidious.
When a company manufactures its own generic, it is not promoting competition - it is strangling it. This practice delays true market entry by independent manufacturers and suppresses price erosion. It is anticompetitive by design.
And to those who say ‘it’s the same drug’ - yes, chemically. But regulatory equivalence does not equate to ethical integrity. We are not merely consumers - we are citizens of a healthcare system that must be protected from predatory consolidation.
Let us not mistake corporate convenience for public good.
Randy Harkins
February 15, 2026 AT 06:33
Love this breakdown! 🙌 Seriously, if you’re on a med that’s been around for a while, always ask about authorized generics. I saved $300 last year just by switching my acid reflux med.
Also, huge shoutout to pharmacists who take the time to explain this stuff - you’re the real MVPs. 💯
Chima Ifeanyi
February 16, 2026 AT 08:58
Let’s not pretend this is about patient care. This is a PBM-driven scheme to shift liability and obscure formulary economics. Authorized generics are a Trojan horse. The brand manufacturers retain control over supply, pricing, and distribution - all while pretending they’re ‘helping’ patients.
And don’t get me started on the NDC code chaos. Pharmacies are still using legacy systems that treat authorized generics as brand-name drugs. That’s not oversight - that’s systemic negligence.
Meanwhile, real generics from independent manufacturers are being sidelined. This isn’t progress - it’s a monopoly with a new label.
Also, the FDA list? Incomplete. Outdated. Not even reliable. You think they’re keeping up with 147 products? Please. Half of them are ghost entries.
Tori Thenazi
February 16, 2026 AT 20:40
Okay, but what if the authorized generic is secretly made in China? I heard a guy on YouTube who said his cousin’s neighbor’s brother works at a warehouse in Shanghai and they’re repackaging brand pills and slapping on ‘authorized generic’ labels…
And what about the inactive ingredients? They’re not regulated the same way! What if I’m allergic to the dye? Or the filler? No one talks about this!
Also - did you know that some authorized generics are made in the same facility as the brand, but on a different shift? What if the machine calibration is off? What if the quality control person was hungover? 😱
And why does the FDA even allow this? Who approved this? Who’s behind this? I think it’s Big Pharma… and maybe the government… and I think they’re using it to track us.
Also - my cousin’s dog got sick after taking one. Coincidence? I think not.
Angie Datuin
February 17, 2026 AT 16:23
My insurance switched me to an authorized generic for my thyroid med last year. I didn’t even notice until I saw the receipt. Saved me $40/month. No side effects. No issues.
Just… wanted to say thanks to whoever wrote this. It’s nice to finally understand what’s going on.
Monica Warnick
February 19, 2026 AT 03:09
I’ve been reading this whole thing and I’m just… confused. So if it’s made by the same company, why isn’t it just called the brand name? Why do we need this whole ‘authorized generic’ label? It’s like they’re trying to trick us into thinking it’s cheaper when it’s basically the same thing.
Also - I read somewhere that they use different dyes in these. What if I’m allergic to red dye? Shouldn’t they be required to tell us? I’m not buying it unless I know exactly what’s inside.
And why does my pharmacy keep giving me different pills? One time it was blue, next time it was white. I’m starting to think they’re swapping them for profit.
Ashlyn Ellison
February 19, 2026 AT 13:53
Just switched to the authorized generic for my birth control. Same pill, half the price. No side effects. Done.
Also - if your pharmacy doesn’t tell you when they switch you, ask them. It’s your right. And if they act like it’s no big deal? They’re not doing their job. You deserve to know what’s in your medicine - even if it’s just a different color.