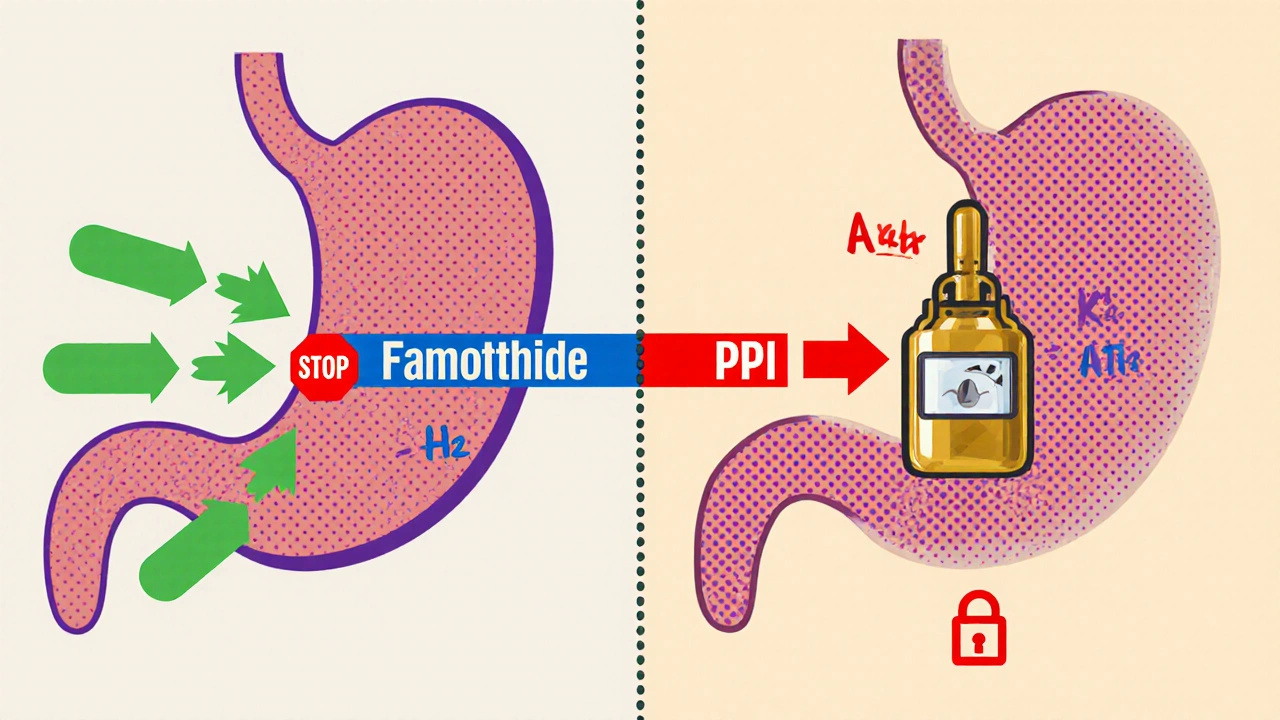
When stomach acid keeps you up at night or burns your chest after a meal, you quickly start looking for relief. Two drug families dominate the market: Famotidine is an H2‑blocker that reduces acid production by targeting histamine receptors, while Proton Pump Inhibitors (PPIs) shut down the final step of acid secretion. Deciding which one fits your lifestyle isn’t just about price - it’s about how fast the drug works, how long it lasts, side‑effect profile, and what your doctor recommends for your specific condition.
What Is Famotidine?
Famotidine belongs to the H2‑receptor antagonist class, often called H2 blockers. It blocks histamine‑2 receptors on the parietal cells of the stomach, which stops one of the primary signals that tells the cells to pump out acid. Because it targets a specific pathway, the drop in acid is moderate but steady.
- Typical adult dose: 20 mg twice daily or 40 mg once daily for heartburn; higher doses (up to 80 mg) are used for ulcer treatment.
- Onset of action: 30-60 minutes.
- Duration: 8-12 hours.
- OTC availability: Yes, in many countries including the UK and US.
Because famotidine is short‑acting, many people take it only when symptoms appear or as a short‑term bridge while waiting for a prescription PPI to kick in.
What Are Proton Pump Inhibitors?
PPIs work downstream of H2 blockers. They bind covalently to the H+/K+ ATPase enzyme - the “proton pump” - located on the stomach’s parietal cells. This irreversible inhibition stops the final step of acid production, leading to a profound and long‑lasting reduction in gastric acidity.
- Common PPIs: omeprazole, esomeprazole, lansoprazole, pantoprazole, rabeprazole.
- Typical adult dose: 20 mg once daily (omeprazole) or 40 mg daily (esomeprazole) for GERD.
- Onset of action: 1-2 hours (full effect may need 3-5 days of continuous use).
- Duration: up to 24 hours; effect lasts longer than plasma half‑life due to irreversible binding.
- OTC availability: Yes, low‑dose versions are sold over the counter in many regions.
PPIs are the go‑to choice for chronic conditions like gastro‑esophageal reflux disease (GERD) because they keep acid levels consistently low.
How Do They Compare in Real‑World Efficacy?
Clinical trials consistently show that PPIs provide superior symptom control for moderate‑to‑severe GERD. A 2023 meta‑analysis of 18 studies reported that 70 % of patients on a PPI achieved complete symptom relief versus 45 % on an H2 blocker like famotidine. However, for occasional heartburn or mild dyspepsia, famotidine works just as well and avoids the higher pill burden of daily PPIs.
If you need fast relief after a big meal, famotidine’s quick onset can be a big plus. PPIs, while more potent, often require a few days of consistent dosing before you feel the full benefit.
Side‑Effect Profiles - What to Watch For
Both drug families are generally safe, but the patterns differ.
| Side Effect | Famotidine | PPIs |
|---|---|---|
| Headache | Common | Common |
| Diarrhea | Rare | Occasional |
| Vitamin B12 deficiency | Very rare | Possible with >1 year use |
| Kidney concerns | Rare (especially in high‑dose) | Rare |
| Rebound acid hypersecretion | Low risk | Higher risk after abrupt discontinuation |
Long‑term PPI use has been linked to increased risk of fractures, Clostridioides difficile infection, and small‑intestine bacterial overgrowth. If you only need short‑term relief, famotidine sidesteps many of those concerns.
Drug Interactions and Metabolism
Famotidine is largely excreted unchanged in the urine, so it has minimal interaction with the cytochrome P450 system. That makes it a safer choice for patients on multiple medications, especially those metabolised by CYP3A4 (e.g., certain statins, antihistamines).
PPIs, on the other hand, are metabolised by CYP2C19 and CYP3A4. They can raise plasma levels of drugs like clopidogrel, warfarin, and some HIV protease inhibitors. Always double‑check with your pharmacist if you’re on a complex regimen.
Cost and Accessibility
In the UK, a pack of 28 × 20 mg famotidine tablets costs around £3-£5, while a similar‑sized pack of a generic PPI (e.g., omeprazole 20 mg) runs about £6-£9. Insurance coverage varies, but most NHS formularies list both as inexpensive first‑line options. If price is a primary driver and you have mild symptoms, famotidine often wins the cost‑effectiveness race.
Special Populations - Who Should Prefer One Over the Other?
- Elderly patients: Kidney function declines with age; dose famotidine carefully (often reduced to 20 mg once daily). PPIs are fine but watch for bone‑density concerns.
- Pregnant women: Both classes are classified as Category B in the UK, but famotidine is sometimes preferred because of its short half‑life.
- Patients with Helicobacter pylori infection: PPIs are essential as part of eradication regimens. Famotidine alone won’t clear the bacteria.
- Those with severe erosive esophagitis: PPIs provide the acid suppression needed to heal tissue.
Decision Guide - How to Pick the Right Drug for You
- Assess symptom severity. Mild, occasional heartburn → start with famotidine. Frequent or severe reflux → consider a PPI.
- Consider timing. Need quick relief after meals? Famotidine’s 30‑minute onset is handy.
- Think about treatment length. If you anticipate only a few weeks of use, famotidine is low‑risk. For chronic GERD, a PPI is usually more effective.
- Review other medications. If you’re on drugs metabolised by CYP enzymes, famotidine may cause fewer interactions.
- Check for underlying conditions. Ulcers, H. pylori, or severe esophagitis demand a PPI.
- Discuss with your clinician. Personal health history (kidney disease, bone health, pregnancy) can tip the balance.
In practice, many doctors start patients on a PPI for a short course (4‑8 weeks), then step down to an H2 blocker like famotidine for maintenance if symptoms stay under control.
Quick Comparison Table
| Attribute | Famotidine (H2 Blocker) | Proton Pump Inhibitors |
|---|---|---|
| Mechanism | Blocks histamine‑2 receptors | Irreversibly inhibits H+/K+ ATPase |
| Onset | 30‑60 minutes | 1‑2 hours (full effect 3‑5 days) |
| Duration of effect | 8‑12 hours | Up to 24 hours |
| Typical OTC dose | 20‑40 mg | Low‑dose (e.g., 10 mg omeprazole) |
| Common side effects | Headache, mild constipation | Headache, diarrhea, potential B12 deficiency |
| Long‑term risks | Low | Fracture risk, C. difficile, rebound acid |
| Drug interaction potential | Minimal | Moderate - CYP2C19/3A4 |
| Cost (UK, 28‑day supply) | £3‑£5 | £6‑£9 |
Bottom Line
If you need fast, on‑demand relief and want to keep medication interactions to a minimum, famotidine is a solid first step. For chronic, severe reflux, or when you’re dealing with ulcer disease, PPIs provide the stronger, longer‑lasting acid suppression that heals the lining.
Remember, self‑medication works best when you know the underlying cause of your symptoms. A short trial of famotidine can tell you whether acid is the main culprit, while a physician‑guided PPI course can manage deeper issues.
Can I switch from a PPI to famotidine without a doctor’s advice?
For most people, stepping down from a PPI to an H2 blocker after symptoms are controlled is safe, but you should still check with a healthcare professional. They can guide you on tapering to avoid rebound acid production.
How long can I take famotidine safely?
Short‑term use (up to 8 weeks) is well established. Longer use is generally considered safe, but the kidneys clear most of the drug, so people with chronic kidney disease should use the lowest effective dose.
Do PPIs cause weight gain?
Weight changes aren’t a direct effect of PPIs. However, if acid reflux is reduced, some people eat larger meals more comfortably, which can lead to gradual weight increase.
Are there natural alternatives to famotidine or PPIs?
Lifestyle tweaks-like raising the head of the bed, avoiding late‑night meals, and limiting caffeine or alcohol-help many people. Herbal options such as deglycyrrhizinated licorice (DGL) or aloe vera juice may soothe the lining, but they don’t suppress acid production like the medications.
What should I do if I experience rebound acid after stopping a PPI?
Gradually taper the dose (e.g., switch to a lower‑strength PPI or add famotidine for a few weeks). This step‑down approach lets the stomach adjust without a sudden surge of acid.

Grace Silver
October 25, 2025 AT 12:40
I see this as a balance between quick relief and long‑term health, where famotidine offers speed and PPIs offer depth
Brett Witcher
October 28, 2025 AT 09:07
From a pharmacological perspective, the irreversible inhibition of the H+\/K+ ATPase by PPIs confers a substantially prolonged acid suppression compared with the reversible H2‑receptor blockade of famotidine.
Abby W
October 31, 2025 AT 06:34
Wow, I totally get the hustle of heartburn after a taco night 🌮💥 famotidine is like that quick‑fire sidekick while PPIs are the superhero that shows up later 😎
Lisa Woodcock
November 3, 2025 AT 04:00
In many Asian cultures we rely heavily on tea and ginger to soothe the gut, but when symptoms get serious a gentle H2 blocker can fit nicely alongside those traditions without clashing with dietary habits.
krishna chegireddy
November 6, 2025 AT 01:27
People don’t tell you that the pharma giants push PPIs so you stay dependent, famotidine is the hidden hero that the system pretends doesn’t exist, and it’s simple enough that anyone can grab it without a big conspiracy swirling around their prescription pad.
kevin burton
November 8, 2025 AT 22:54
Let me break this down in plain terms. Famotidine works by blocking histamine receptors on the stomach lining, which cuts down acid production fairly quickly, usually within half an hour. Because it’s a reversible blocker, the effect wears off after about eight to twelve hours, so you can take it as needed for occasional heartburn. This makes it a good choice for people who only have sporadic symptoms or who want to avoid the heavier side‑effect profile of long‑term acid suppression.
PPIs, on the other hand, target the final step of acid secretion by irreversibly inhibiting the proton pump. That’s why they provide a much deeper reduction in gastric acidity, but also why they need a few days of consistent dosing before you notice the full benefit. Once the pump is blocked, the effect lasts up to 24 hours even though the drug’s half‑life in the blood is short.
From a safety standpoint, both classes are generally well tolerated. Famotidine has minimal drug‑drug interactions because it’s cleared unchanged in the urine. PPIs are metabolized by liver enzymes CYP2C19 and CYP3A4, which can raise levels of certain medications like clopidogrel or some statins. Long‑term PPI use has been linked to nutrient deficiencies, bone fractures, and an increased risk of certain infections, so it’s best reserved for chronic or severe GERD.
Cost is another factor. In the UK a month's supply of famotidine is usually under £5, while a generic PPI runs about £6‑£9. If you’re on a tight budget and your reflux is mild, famotidine often wins on price.
Bottom line: use famotidine for quick, on‑demand relief or as a short‑term bridge, and consider a PPI if you need consistent acid control for an extended period or have complications like erosive esophagitis.
Max Lilleyman
November 11, 2025 AT 20:20
Nice summary, but famotidine is just a placebo.
Shannon Stoneburgh
November 14, 2025 AT 17:47
That’s a harsh take; the evidence shows famotidine works for many people, especially when used correctly.
Terell Moore
November 17, 2025 AT 15:14
Ah, the classic “quick fix vs. deep dive” debate – truly a reflection of our society’s love for shortcuts over sustained effort, isn’t it?
Corrine Johnson
November 20, 2025 AT 12:40
Indeed, the discourse must perpetually oscillate between superficial immediacy, and the profound, deliberate, and methodical pursuit of lasting remission; otherwise, we risk succumbing to the very trivialities we so vehemently disdain.
Jennifer Stubbs
November 23, 2025 AT 10:07
The points raised are solid, but it would help to see more real‑world examples of patients transitioning from PPIs to famotidine without rebound symptoms.