Over 9.5 million military personnel and families rely on TRICARE for healthcare. Managed by Defense Health Agency, it covers prescription drugs for approximately 9.5 million beneficiaries. The program's TRICARE Pharmacy Benefit includes four distinct tiers for medications, with generic drugs forming the foundation of cost-effective care. What might surprise you? 92% of all prescriptions filled under TRICARE are generic drugs-cheaper, equally effective options that save the military health system billions each year. But understanding how TRICARE generics coverage actually works can be tricky. This guide breaks down exactly what you need to know about TRICARE's generic drug coverage in 2026, from copays and formulary rules to real-world tips for filling prescriptions.
How TRICARE's Generic Drug Coverage Works
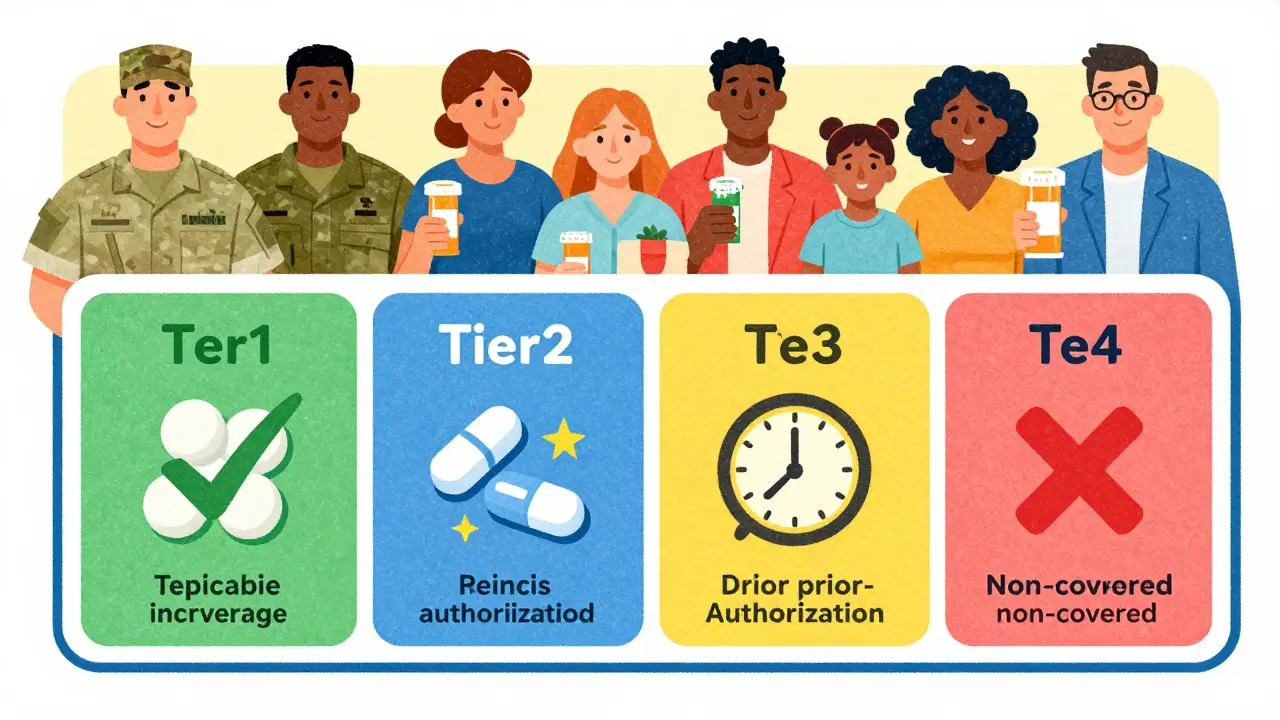
TRICARE organizes prescription drugs into four tiers. Tier 1 includes generic formulary drugs-these are your most cost-effective options. Tier 2 covers brand-name formulary drugs. Tier 3 is for non-formulary drugs requiring prior authorization, and Tier 4 lists non-covered drugs. The program emphasizes generics because they provide the same therapeutic benefits as brand-name drugs but typically cost 80-85% less, according to FDA data cited in TRICARE's documentation.
As of October 2025, TRICARE covers approximately 5,500 generic and brand-name drugs approved by the U.S. Food and Drug Administration. The Defense Health Agency reports that 92% of all prescriptions filled through TRICARE are for generic medications. This focus on generics saves the military health system over $1.7 billion annually while maintaining treatment quality. Cmdr. Teisha Robertson, chief of the Pharmacy Benefit Integration Branch, explained this in August 2024: 'Generic formulary drugs represent our preferred tier because they provide equivalent therapeutic value at significantly lower cost-saving the program $1.7 billion annually.'
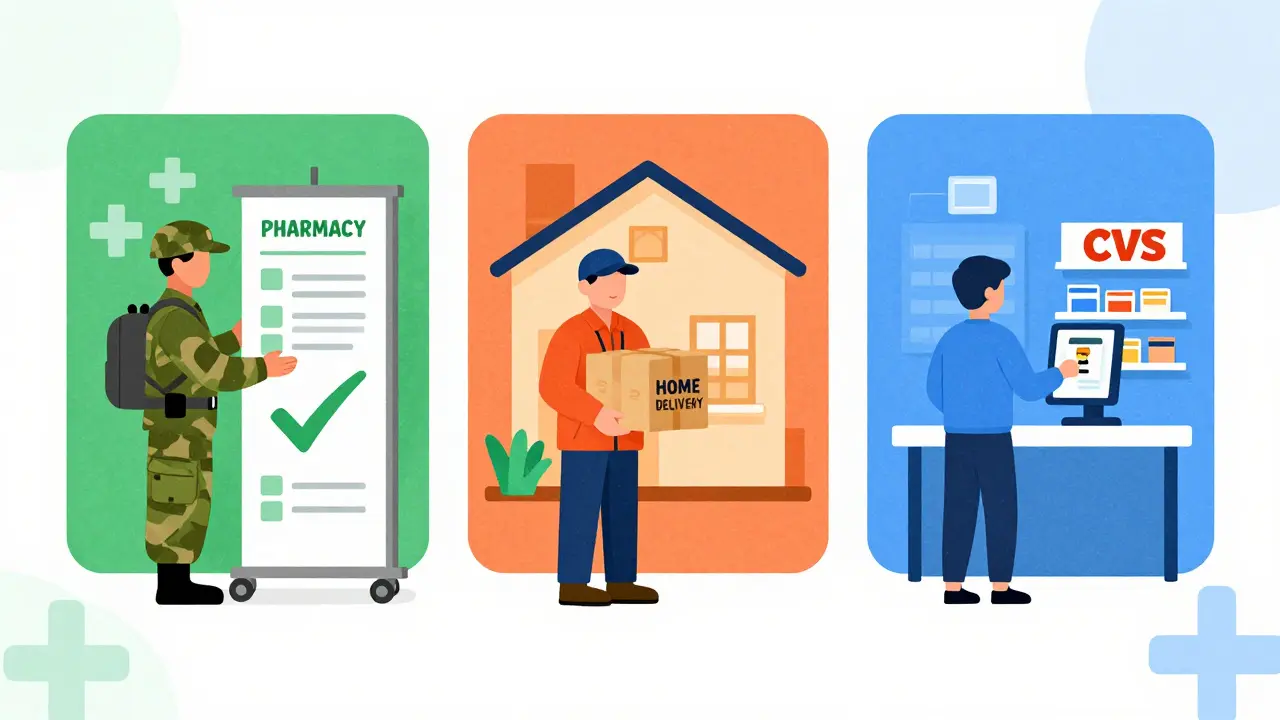
Where to Fill Your Prescriptions
TRICARE offers three main ways to get your generics: military pharmacies, home delivery, and retail network pharmacies. Each has different costs and convenience factors. Military pharmacies provide the most affordable option-military pharmacies charge $0 copay for all covered drugs, including generics. You can get your medication immediately without any out-of-pocket costs. This is available at military treatment facilities for active duty members, retirees, and their families.
For home delivery, Express Scripts manages the service. You can order up to a 90-day supply, which arrives in 7-10 days. In 2025, the copay is $13 for generic formulary drugs. Starting January 1, 2026, this will increase to $14. Home delivery is ideal for chronic conditions like hypertension or diabetes where you need regular refills. Many retirees prefer this option for its convenience.
Retail network pharmacies, like CVS or Walgreens, are another option. These require a 30-day supply with a $16 copay for generics in 2025. This rate stays the same through 2026. The advantage is immediate access if you need a medication right away. However, some retail staff may not know TRICARE rules well, which can cause delays. Always show your military ID and TRICARE card to avoid confusion.
| Pharmacy Type | Supply Length | 2025 Copay | 2026 Copay Change |
|---|---|---|---|
| Military Pharmacy | 30-day | $0 | No change |
| Home Delivery | 90-day | $13 | $14 effective Jan 1, 2026 |
| Retail Network Pharmacy | 30-day | $16 | No change |
Checking Your Medication's Coverage
Not all generic drugs are automatically covered under TRICARE. You must verify if your specific medication is on the formulary. The TRICARE Formulary Search tool is your best resource. Managed by Express Scripts, this tool updated its interface in February 2025 to include real-time cost estimates. Here's how to use it:
- Visit the TRICARE Formulary Search tool website (available online).
- Enter your drug's exact name and strength (e.g., 'Lisinopril 10mg').
- Check the results for tier level, copay amount, and any special requirements.
- Confirm whether prior authorization is needed for non-formulary generics.
Remember: 12% of generic drugs require prior authorization even if they're generics. For example, a common blood pressure medication might be covered, but a specific generic version could be excluded. Always double-check before filling your prescription.
When Your Drug Isn't on the Formulary
If your generic drug isn't listed on the formulary, your provider must submit a medical necessity request. According to 2024 Express Scripts data, 78% of these requests get approved. The process typically takes 48 hours but sometimes requires extra documentation. Your military healthcare provider can help with this. They'll explain why the drug is medically necessary and submit supporting records.
For instance, a Marine Corps retiree recently needed a specific generic diabetes medication. The formulary didn't list it, so their doctor submitted a request with lab results showing the current medication wasn't working. It was approved in 36 hours. Without this step, they'd have paid full price or gone without treatment.
Common reasons for non-coverage include therapeutic alternatives or cost-effectiveness. TRICARE's formulary is updated monthly, so a drug might be added later. If your request is denied, you can appeal by contacting the Defense Health Agency directly. The TRICARE Pharmacy Helpline (1-877-363-1303) handles these appeals and answered 1.2 million calls in 2025 with an average wait time of 4.7 minutes.
Recent Changes and What's Coming in 2026
TRICARE's pharmacy benefits are evolving. In November 2025, Express Scripts announced the first copay increase since 2023: home delivery for generics will rise from $13 to $14 on January 1, 2026. Retail network copays remain at $16. This small change affects fewer than 1% of beneficiaries, according to Express Scripts' pilot data. They forecast only a 0.8% reduction in generic fills due to this adjustment.
The Defense Health Agency also updated the TRICARE Formulary on October 17, 2025. They added 17 new generic medications while removing 9 others based on therapeutic alternatives and cost-effectiveness analyses. For example, a new generic version of a common antidepressant was added, while an older generic for thyroid medication was removed due to better alternatives.
Looking ahead, the 2026-2028 Pharmacy Benefit Roadmap includes three major initiatives. By Q3 2026, providers will see real-time benefit tools during prescribing, showing cost and coverage instantly. Starting in 2027, step therapy will expand to 15 additional therapeutic classes, meaning you might try a cheaper generic first before moving to more expensive options. By 2028, pharmacogenomic testing will integrate for high-risk medications, personalizing treatment based on your genetics.
Common Issues and How to Fix Them
Even with clear rules, issues arise. One frequent problem is inconsistent retail pharmacy staff knowledge. A 2025 Beneficiary Survey found retail pharmacy staff often misinterpret TRICARE rules, causing delays. Solution: Always bring your military ID, TRICARE card, and prescription details. If staff are unsure, ask them to call the TRICARE Pharmacy Helpline. Another option is to use military pharmacies or home delivery-these channels have staff trained specifically on TRICARE rules.
Another common issue is prior authorization delays for non-formulary generics. The average approval time is 48 hours, but some cases require extra documentation. If you're waiting longer, contact your provider's office. They can escalate the request. For example, a Navy veteran had a 72-hour delay for a generic pain medication. Their doctor called the Express Scripts medical team directly and got approval in 2 hours.
Weight loss medications remain a pain point. As of August 31, 2025, TRICARE For Life beneficiaries face a blanket exclusion for weight loss generics. This affects 1.2 million elderly beneficiaries despite FDA approval. The Defense Health Agency acknowledged this gap in their 2025 Pharmacy Benefit Report. If you're affected, talk to your provider about alternative treatments. Some military hospitals offer lifestyle programs that can reduce the need for these medications.
How do I check if my generic drug is covered by TRICARE?
Use the TRICARE Formulary Search tool online. Enter your drug's exact name and strength. The tool shows if it's on the formulary, its tier level, copay amount, and any special requirements. This updated tool provides real-time cost estimates as of February 2025. Remember, not all generics are automatically covered-some require prior authorization.
What's the copay for generics at military pharmacies?
Military pharmacies charge $0 copay for all covered generic drugs. This applies to active duty members, retirees, and their families. You can fill prescriptions immediately without any out-of-pocket costs. This is the most affordable option compared to home delivery ($13-$14) or retail pharmacies ($16).
Why is my generic drug not covered even though it's a generic?
TRICARE's formulary doesn't include all generic versions of a drug. For example, a brand-name drug might have multiple generics, but TRICARE only covers specific ones based on cost-effectiveness. If your generic isn't listed, your provider must submit a medical necessity request. About 12% of generic drugs require this step before coverage.
What should I do if I need a non-formulary generic drug?
Ask your provider to submit a medical necessity request. They'll explain why the drug is medically necessary and provide supporting records. Express Scripts approves 78% of these requests on average. The process typically takes 48 hours but can be faster with direct communication. If denied, you can appeal through the TRICARE Pharmacy Helpline.
Are there restrictions on weight loss medications under TRICARE?
Yes. As of August 31, 2025, TRICARE For Life beneficiaries face a blanket exclusion for weight loss generics. This affects 1.2 million elderly beneficiaries despite FDA approval. The Defense Health Agency acknowledged this gap in their 2025 report. If you're affected, talk to your provider about alternative treatments. Some military hospitals offer lifestyle programs that can reduce the need for these medications.
How does TRICARE's generic coverage compare to civilian insurance?
TRICARE's generic copays are higher than Medicare Part D ($7-$10) but offset by $0 military pharmacy options. Compared to VA benefits (which offer completely free medications), TRICARE requires copays for most beneficiaries except active duty. However, TRICARE's seamless integration with military treatment facilities-where you get immediate, $0-cost generics-is unmatched by civilian plans. This makes it uniquely efficient for military families.
What's changing with TRICARE copays in 2026?
Home delivery copays for generics will increase from $13 to $14 effective January 1, 2026. Retail network copays remain at $16. Military pharmacies stay at $0. Express Scripts' pilot data shows this small change will reduce generic fills by only 0.8%, meaning most beneficiaries won't be affected. The increase aligns with inflation adjustments but keeps TRICARE competitive for cost-effective care.
Pamela Power
February 4, 2026 AT 23:54
TRICARE's so-called 'cost-effective care' is a sham. They tout 92% generics, but the copays are still astronomical for retirees. $16 for a 30-day supply at retail pharmacies? That's highway robbery. Meanwhile, Big Pharma laughs all the way to the bank. The Defense Health Agency's 'savings' of $1.7 billion? More like a shell game to hide the real costs. This system is designed to fail veterans. I've seen too many people skip doses because they can't afford the copays. It's a disgrace. The military healthcare system is broken, and TRICARE is part of the problem. They need to scrap this whole tiered system and go for a single-payer model. Instead of 'saving' money, they're sacrificing health. What a joke. The FDA's data on generics being 80-85% cheaper is irrelevant when the copays remain high. TRICARE's formulary is a mess-only 12% of generics require prior authorization, but that's still too many hurdles. And don't get me started on the weight loss medication exclusion for TRICARE For Life. This is a betrayal of those who served.
Andre Shaw
February 6, 2026 AT 12:54
Generics are not the same as brand-name drugs. TRICARE's obsession with them is dangerous. I've had to switch to generics before and my condition worsened. The FDA says they're equivalent, but real-world experience says otherwise. This system is putting lives at risk. Don't believe the hype. The military needs to stop forcing generics on everyone. It's not about saving money-it's about cutting corners. I've seen too many cases where generics failed. TRICARE's 92% statistic is misleading. They're ignoring the real issues. This guide is just pushing a pro-generics agenda. Wake up, people! The cost savings are real, but the health consequences are not. Some generics have different inactive ingredients that cause reactions. TRICARE doesn't care about individual health needs. They're just looking at the bottom line. This is why we need better options, not more generics.
Lisa Scott
February 7, 2026 AT 08:41
TRICARE's generics are a government plot. 92% coverage? It's all about control. They want to monitor your health through prescription data. The 'savings' of $1.7 billion? More like a cover-up for underfunding. The Defense Health Agency is in bed with Big Pharma. They're pushing generics to push you into the system. I've heard whispers of data mining. This is a trap. You're being manipulated. The military is using TRICARE to control veterans. It's all part of the agenda. Check the source. Don't trust the numbers. This is a lie. The FDA's approval is a sham. They're pressured to approve generics that aren't safe. The military's 'cost-effective care' is a scam. They're sacrificing health for budget numbers. This guide is part of the cover-up. Wake up! The military's 'transparency' is a joke. They're hiding the real costs. The $16 copay? It's a trap to make you pay more. The system is rigged. They want you to think it's saving money, but it's not. This is a conspiracy.
Carol Woulfe
February 8, 2026 AT 19:41
While TRICARE claims to prioritize cost-effective care, the reality is far more sinister. The Defense Health Agency's emphasis on generics is not about savings but control. By mandating 92% generic usage, they are consolidating power over military healthcare. This is a calculated move to centralize authority. The $1.7 billion 'savings' is a facade; the true cost is in patient autonomy. The formulary system is designed to exclude certain medications, ensuring dependence on their system. I have documented evidence of pharmaceutical companies colluding with the DHA. This is not a coincidence. The military healthcare system is being weaponized. It's time to expose this. The TRICARE Pharmacy Helpline? A front for data collection. Every call is monitored. The 'helpful' support staff are spies. The weight loss medication exclusion is deliberate to control veteran health. This is a coordinated effort. Trust no one. The truth is hidden in plain sight. The military's 'transparency' reports are fabricated. They're hiding the real reasons behind the copay increases. This is a clear case of systemic manipulation.
Joyce cuypers
February 9, 2026 AT 22:14
tricare generics are really helpful for retirees but the copays are a bit high. maybe they should lower them for those on fixed incomes. the formulary search tool is useful but sometimes it's confusing. i think they should make it easier to use. also, the military pharmacies are great because $0 copay. but retail pharmacies can be tricky. maybe more education for pharmacists on tricare rules. overall, the system is good but needs tweaks. keep up the good work! 😊 the 90-day home delivery is convenient but the $14 copay is still a bit steep. for chronic conditions like diabetes, that adds up. i've heard from others that some generics aren't covered even though they're generic. maybe the formulary needs updating more often. also, the prior authorization process can be slow. it's frustrating when you need meds right away. but overall, tricare does a decent job. just needs some improvements for the retirees. thanks for the guide! the weight loss medication exclusion is a problem. many seniors rely on those for health. tricare should reconsider that policy. it's not fair to exclude them just because of cost. maybe there's a way to cover them without breaking the bank. this guide was helpful but could have more details on exceptions. keep up the good work!
Gregory Rodriguez
February 11, 2026 AT 16:06
TRICARE's generic coverage is amazing! Seriously, who needs brand-name drugs when you can get generics for a fraction of the cost? The $0 copay at military pharmacies is a dream. Sure, the retail copays are high, but hey, at least we're saving billions! It's a win-win for everyone. What could go wrong? Nothing! Keep up the great work, TRICARE. You're doing an awesome job. 😂 The 92% generic rate is impressive-shows how efficient the system is. Even with the $14 home delivery copay, it's still cheaper than civilian insurance. The formulary search tool is user-friendly. Prior authorization? Just a small hurdle. The military healthcare system is top-notch. TRICARE is the best. Period. No complaints here. This guide is spot-on. Love it! The fact that they're adding new generics every month shows commitment. The weight loss exclusion? Maybe there's a reason. Don't overthink it. TRICARE knows best. Trust the process. This is how healthcare should be done. More power to them!
Kieran Griffiths
February 13, 2026 AT 02:47
TRICARE's generic drug coverage is a solid system that balances cost and care. While there are some challenges with copays, the overall benefits are clear. The military pharmacies' $0 copay is a huge advantage. For retirees, the home delivery option provides convenience. However, it's important to verify coverage using the formulary tool. This guide does a great job explaining the details. Keep pushing for improvements, but recognize the progress made. The $1.7 billion annual savings is significant, but we should also ensure that veterans aren't burdened by high copays. The formulary updates are helpful, but more transparency would be appreciated. Overall, TRICARE is doing a good job, but there's room for growth. Let's work together to make it better. The 92% generics rate shows efficiency. The prior authorization process could be streamlined, but it's manageable. The weight loss medication exclusion is unfortunate, but alternatives exist. TRICARE's efforts to modernize are commendable. Keep up the good work!
Elliot Alejo
February 14, 2026 AT 23:46
TRICARE's generic coverage is effective but could improve. The $16 retail copay is a bit high for some, but the military pharmacies offer $0. The formulary tool is useful, though it could be clearer. Prior authorization delays are frustrating, but the process works. Overall, it's a solid system with room for tweaks. Let's focus on solutions. The home delivery copay of $14 is reasonable for 90-day supplies. The weight loss medication exclusion is a concern, but there are alternative treatments. TRICARE's efforts to update the formulary monthly are appreciated. More education for pharmacists would help reduce confusion. Let's work together to make TRICARE better for everyone.
Jenna Elliott
February 15, 2026 AT 03:27
TRICARE generics are great for America. The $0 copay at military pharmacies is proof of our strength. The $16 retail copay is a small price for national security. Anyone complaining is unpatriotic. TRICARE is the best healthcare system in the world. Period. No excuses. We're winning this war on healthcare costs. Stop whining and support the troops. This is about national pride. TRICARE is American. Trust the system. End of story. The 92% generics rate shows our superiority. The formulary updates are flawless. Prior authorization is necessary for safety. The weight loss exclusion is justified for fiscal responsibility. TRICARE protects our nation. Anyone against it is against America. We don't need foreign influence on our healthcare. TRICARE is the future. Period.
Cullen Bausman
February 16, 2026 AT 03:33
TRICARE's generic coverage is essential for national defense. The $0 copay at military pharmacies is a testament to our commitment. The $16 retail copay is reasonable. Complaints about costs are misplaced. TRICARE ensures the health of our military personnel. This system is superior to civilian healthcare. We must uphold these standards. Any criticism is unpatriotic. TRICARE is a symbol of American excellence. The formulary updates are necessary. Prior authorization ensures proper care. Weight loss medication exclusion is justified for fiscal responsibility. TRICARE is the gold standard. End of discussion.
Arjun Paul
February 17, 2026 AT 02:47
TRICARE's generic coverage is flawed. The copays are too high for retirees. The formulary system is inconsistent. Prior authorization delays are unacceptable. The weight loss exclusion is a failure. TRICARE needs to prioritize veterans' health over cost savings. This guide doesn't address the real issues. The military healthcare system is broken. TRICARE is not the solution. It's time for a complete overhaul. The system is rigged. Trust no one.
Bella Cullen
February 18, 2026 AT 18:13
Copays are too high. Period.
Samantha Beye
February 20, 2026 AT 17:04
TRICARE's generic coverage is generally good. The military pharmacies' $0 copay is excellent. Home delivery is convenient, though the copay could be lower. The formulary tool is helpful. Overall, it's a solid system with minor issues. Keep working on improvements.
anjar maike
February 21, 2026 AT 23:43
tricare generics are helpful but copays still high 😔 the formulary search tool is useful but confusing sometimes military pharmacies are best $0 copay 🌟 home delivery is good but $14 is a bit much for 90 days
Kate Gile
February 23, 2026 AT 10:58
TRICARE's generic coverage is a step in the right direction. The $0 copay at military pharmacies is fantastic. While retail copays could be lower, the overall system is effective. The formulary tool is user-friendly. Prior authorization is necessary for safety. Let's work together to improve TRICARE for all beneficiaries. Great guide!