Eating Disorders: Signs, Treatment, and Practical Recovery Steps
Eating disorders are more than food or weight — they’re serious mental and physical health conditions. If you’re worried about yourself or someone else, you need clear, practical steps you can take right now. This page gives simple signs to watch for, immediate safety actions, and realistic paths to recovery.
Spotting the warning signs
Early detection matters. Watch for changes in behavior, mood, and physical health. Common red flags include: dramatic weight loss or gain, rigid rules around food, skipping meals, secretive eating, binge episodes followed by vomiting or laxative use, fixing mirrors and clothes, obsession with calories or exercise, social withdrawal, mood swings, and frequent dizziness or fainting.
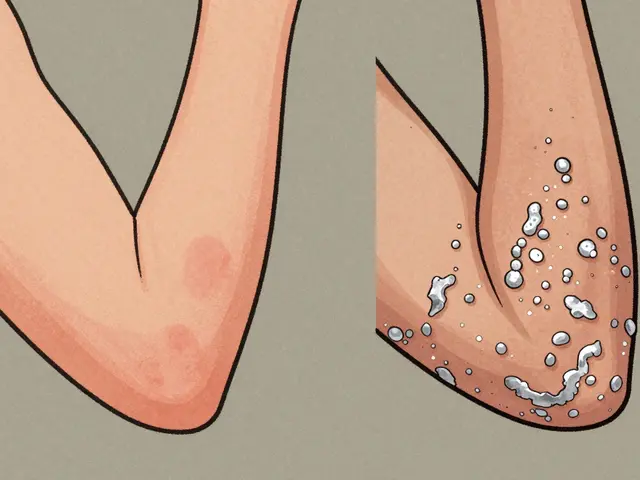
Physical clues can show up too: thinning hair, brittle nails, dental erosion (from vomiting), irregular periods, low blood pressure, cold intolerance, and swelling in hands or feet. If you see a combination of these signs, don’t wait.
Practical next steps and treatment options
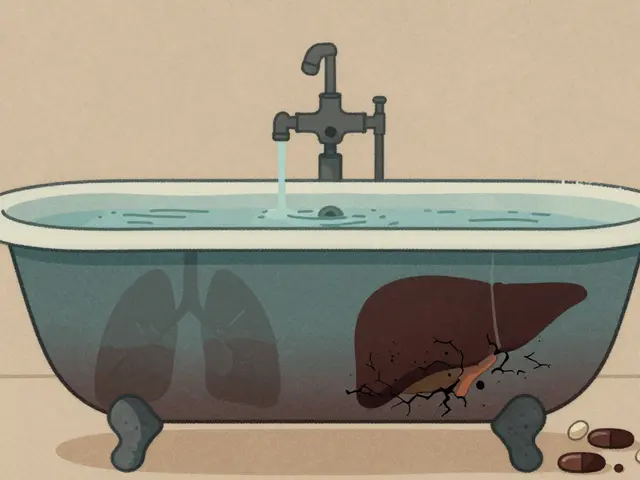
If there’s immediate danger — suicidal thoughts, fainting, severe chest pain, severe dehydration, or inability to keep food down — call emergency services or go to the nearest emergency room. For non-emergencies, start with a trusted primary care doctor. A GP can run basic blood tests, check vitals, and refer you to eating disorder specialists, therapists, and dietitians.
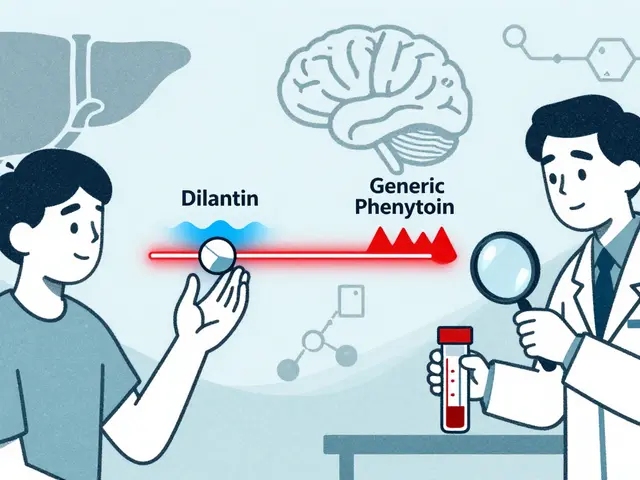
Treatment usually combines three things: medical monitoring, structured nutrition plans, and therapy. Cognitive Behavioral Therapy (CBT) and Family-Based Therapy (FBT) are proven approaches. Dietitians help rebuild safe eating habits and correct nutrient deficits. Sometimes medication helps with anxiety, depression, or binge eating — but meds aren’t a cure by themselves.
Small, practical actions help recovery every day: set simple meal plans, avoid calorie counting apps, keep a food and mood log to spot triggers, and replace rigid dieting language with neutral food talk. Celebrate tiny wins — even one balanced snack or one honest conversation matters.
Family and friends can make a big difference. Offer calm support, avoid blaming or giving unsolicited diet tips, help find appointments, and sit with meals if that’s asked for. If you’re supporting someone who resists help, focus on safety and keep lines of communication open rather than forcing change.
Recovery is rarely linear. Expect setbacks and plan for them: identify triggers, list coping strategies (breathing, short walks, calling a friend), and keep emergency contacts handy. Peer support groups and trusted online communities can reduce isolation, but verify their reliability and avoid content that glamorizes symptoms.
If you need guidance on medications, supplements, or how treatments interact with other health issues, use reliable medical resources or ask a pharmacist or doctor. Medipond.com offers clear information on medicines and treatments if you want trustworthy drug guides and safety tips.
Want help finding local services or a therapist? Start with your GP, local mental health clinics, or national eating disorder helplines. Asking for help is a strong, practical first step — it can save your life and get you back to living without food ruling your day.