DVT (Deep Vein Thrombosis) — what to watch for and what to do
A blood clot in a deep vein—usually in the calf or thigh—can start quietly and suddenly become dangerous. That’s DVT. You don’t always feel drama up front, but a few clear signs and simple actions make a big difference.
Signs & when to act
Watch for one-sided leg swelling, pain or tenderness that gets worse when you stand or walk, warmth, and skin that looks red or darker than the other leg. Those are the common clues. If you suddenly feel short of breath, chest pain, lightheaded or coughing up blood, call emergency services right away—those could mean the clot has moved to your lungs (pulmonary embolism).
If symptoms are milder—swelling, aching, or a tight feeling—contact your doctor the same day. They’ll usually order a leg ultrasound and may do a D-dimer blood test to check for clot activity.
Common causes and real risks
DVT risk goes up after long immobility (long flights or bed rest after surgery), major surgery, recent trauma, active cancer, pregnancy and the weeks after delivery, hormone pills or some fertility treatments, obesity, and smoking. Age matters too—risk rises as you get older. Genetics can also play a role if clotting conditions run in your family.
Not all swelling is DVT. Heart or kidney issues, infections, and chronic venous insufficiency can look similar. That’s why a quick check with a clinician matters.
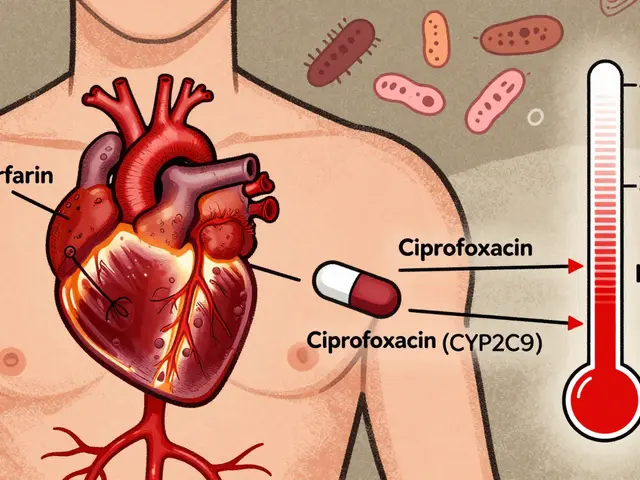
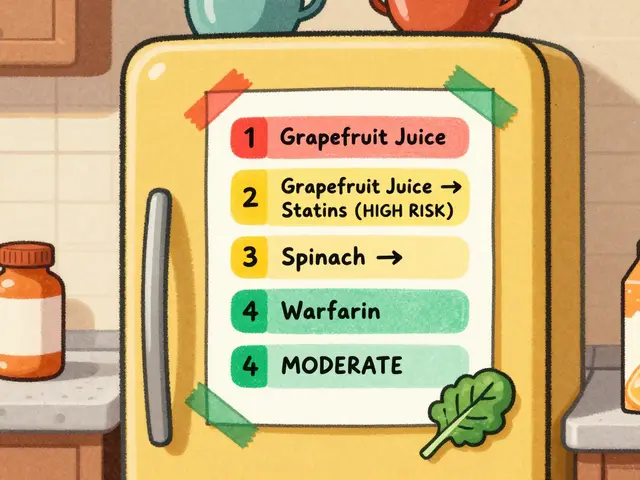
Treatment usually means blood thinners (anticoagulants) like low-molecular-weight heparin, warfarin or direct oral anticoagulants (apixaban, rivaroxaban). Doctors pick the drug and duration based on why the clot happened and your bleeding risk. Compression stockings can ease symptoms and help prevent post-thrombotic pain and swelling. In rare emergency cases, clots may be removed or an inferior vena cava (IVC) filter considered.
Simple prevention helps a lot: move around on long trips (get up every hour on flights, flex ankles), wear compression stockings if advised, stay hydrated, maintain a healthy weight, and follow post-surgery advice on early walking and blood-thinner prescriptions. Avoid combining NSAIDs and blood thinners without medical advice—bleeding risk rises.
If you use online pharmacies, be careful—blood thinners are prescription drugs. Always use a verified pharmacy that requires a prescription and keeps medical records. If you’re unsure, talk with your doctor or pharmacist first.
Keep follow-up appointments after a DVT. Your doctor will monitor therapy, check for bleeding problems, and decide how long you need treatment. If you ever feel new chest pain or shortness of breath, get urgent help.
Want more on related meds, heart health, or buying prescriptions safely? Browse our DVT tag posts for guides on medicines, safe online pharmacies, and heart meds that matter after a clot.