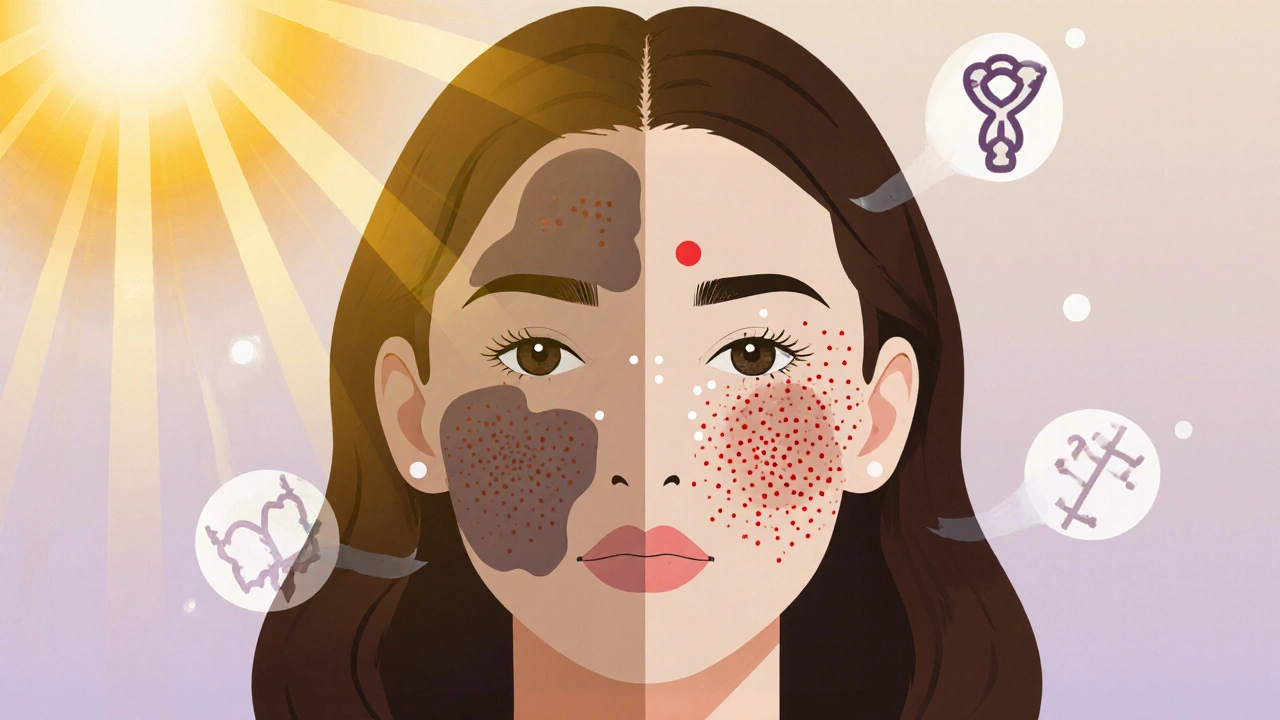
Dealing with melasma and acne at the same time can feel like fighting two battles on the same front line. One condition brings stubborn brown patches, the other erupts with red pimples, and the overlap often leaves you unsure which product will help-or hurt-your skin. This guide breaks down the science, the triggers, and the step‑by‑step routine that lets you treat both without compromising either.
What Is Melasma?
Melasma is a chronic hyperpigmentation disorder that produces symmetrical brown‑gray patches, most commonly on the cheeks, forehead, and upper lip. Hormonal fluctuations, sun exposure, and genetics are the main culprits. While it’s not painful, melasma can be emotionally draining because the discoloration is highly visible.
What Is Acne?
Acne is an inflammatory skin condition that forms when pores become clogged with oil, dead skin cells, and bacteria, leading to blackheads, whiteheads, papules, pustules, and sometimes cysts. Hormones, stress, diet, and certain medications can trigger flare‑ups.
Why They Often Appear Together
- Hormonal overlap: Both conditions respond to estrogen, progesterone, and androgen spikes, which explains why many women notice melasma worsening during pregnancy or while on oral contraceptives.
- Sun exposure: UV rays stimulate melanin production (worsening melasma) and increase sebum, creating a perfect storm for acne.
- Inflammation: Inflammatory acne lesions can leave post‑inflammatory hyperpigmentation that mimics melasma, making differentiation tricky.
Key Principles for Dual Management
- Gentle, non‑comedogenic formulas-avoid heavy occlusives that can choke pores.
- Broad‑spectrum sunscreen every morning-protects against melasma progression and reduces acne‑inducing inflammation.
- Targeted actives that address both pigment and excess oil without causing irritation.
- Consistency over intensity-steady use of mild agents beats occasional strong treatments that trigger flare‑ups.

Topical Agents That Work for Both
| Ingredient | Primary Action | Benefits for Melasma | Benefits for Acne |
|---|---|---|---|
| Azelaic Acid (15‑20%) | Anti‑inflammatory & tyrosinase inhibitor | Reduces melanin production, fades brown patches | Kills P. acnes, normalizes keratinization |
| Niacinamide (5%) | Barrier support & melanosome transfer inhibitor | Lightens hyperpigmentation, improves skin tone | Regulates sebum, reduces redness |
| Retinoids (low‑dose adapalene) | Cell turnover promoter | Speeds pigment clearance | Unclogs pores and prevents new lesions |
| Vitamin C (10‑15% L‑ascorbic acid) | Antioxidant & collagen booster | Inhibits melanin synthesis, brightens skin | Reduces oxidative stress that can aggravate acne |
| Sunscreen (SPF 30‑50, zinc oxide/titanium dioxide) | UV filter | Prevents melasma darkening | Minimizes UV‑induced inflammation |
Building a Daily skin care Routine
Morning:
- Cleanse with a gentle, sulfate‑free foaming wash (pH 5.5) to remove excess oil without stripping the barrier.
- Apply a vitamin C serum (preferably stabilized) to start the brightening process.
- Follow with a thin layer of azelaic acid if you tolerate it; otherwise, use niacinamide.
- Finish with a broad‑spectrum sunscreen that is labelled non‑comedogenic.
Evening:
- Double‑cleanse if you wore makeup or heavy sunscreen: first a micellar water, then the same gentle cleanser.
- Apply a low‑dose retinoid (adapalene 0.1% works for most) on non‑active acne days; skip on breakout nights to avoid irritation.
- Use a moisturizer containing ceramides and hyaluronic acid to restore barrier function.
When Topicals Aren’t Enough: Oral Options
- Oral contraceptives (combined estrogen‑progestin) can stabilize hormonal fluctuations, often improving both melasma and acne. Choose a low‑androgenic progestin to minimize side effects.
- Spironolactone (50‑100 mg daily) blocks androgen receptors, useful for adult women with persistent acne and melasma.
- Tranexamic acid (500 mg twice daily) has shown promise in melasma reduction and may indirectly help acne by reducing inflammation.
Always discuss oral therapy with a dermatologist or GP, as blood work and monitoring may be required.
Lifestyle Tweaks That Make a Difference
- Sun protection beyond sunscreen: Wear wide‑brim hats, seek shade, and avoid peak UV hours (10 am‑2 pm).
- Dietary considerations: Limit high‑glycemic foods and dairy, which can spike insulin and aggravate both conditions.
- Stress management: Practice mindfulness, yoga, or regular exercise-stress hormones can flare acne and worsen melasma.
- Sleep hygiene: Aim for 7‑9 hours; poor sleep disrupts the skin’s repair cycle.
Do’s and Don’ts Quick Guide
- Do patch‑test new actives for at least 48 hours before full use.
- Do keep your pillowcases and phone screens clean to reduce bacterial transfer.
- Don’t over‑exfoliate-excessive physical scrubs can worsen hyperpigmentation.
- Don’t skip sunscreen even on cloudy days; UV‑A penetrates clouds.
When to Seek Professional Help
If you notice any of the following, book a dermatologist appointment:
- Rapid expansion of melasma patches despite diligent sunscreen use.
- Acne nodules or cysts that are painful or leave deep scars.
- Persistent redness, swelling, or signs of infection.
- Desire for procedural treatments (chemical peels, laser, microneedling) that require medical supervision.
Quick Checklist for Managing Both Conditions
- Use a gentle, pH‑balanced cleanser twice daily.
- Apply vitamin C in the morning, retinoid at night (if tolerated).
- Incorporate azelaic acid or niacinamide for dual action.
- Never skip broad‑spectrum sunscreen.
- Consider oral hormonal therapy only under medical advice.
- Monitor diet, stress, and sleep patterns.
Frequently Asked Questions
Can I use benzoyl peroxide for acne if I have melasma?
Benzoyl peroxide is effective for acne, but it can be irritating and may darken melasma patches. If you need it, apply only on breakout areas and keep it away from pigmented zones. Pair it with a soothing moisturizer and sunscreen.
Is it safe to combine retinoids with azelaic acid?
Yes, the combination is often recommended because azelaic acid calms retinoid‑induced irritation while both promote pigment fade and pore clearance. Start with alternate nights, then gradually move to daily use if your skin tolerates it.
How often should I exfoliate when I have both conditions?
Limit chemical exfoliation (AHA/BHA) to 2‑3 times per week. Over‑exfoliating can trigger inflammation, worsening both acne and melasma. Stick to gentle, pH‑balanced formulas.
Do diet changes really affect melasma?
Diet alone won’t cure melasma, but reducing high‑glycemic foods and dairy can lower insulin spikes that aggravate acne and may indirectly reduce melasma flare‑ups caused by inflammation.
Should I consider laser treatment for melasma if I also have active acne?
Laser resurfacing can improve melasma but may inflame active acne, leading to post‑inflammatory hyperpigmentation. Treat acne first, then discuss laser options with a dermatologist once the skin is calm.
alex montana
October 18, 2025 AT 19:58
Wow!!! This post hits all the right notes, and I can’t help but feel the weight of every single detail, the way you balanced melasma and acne like a tightrope‑walker, it’s just… magnificent!!!
Wyatt Schwindt
October 29, 2025 AT 08:41
I appreciate the thorough guide; it’s practical.
Lyle Mills
November 8, 2025 AT 22:24
The regimen wisely incorporates keratinocyte turnover agents, sebum regulation via niacinamide, and melanocyte inhibition through azelaic acid, providing a synergistic protocol.
Barbara Grzegorzewska
November 19, 2025 AT 12:06
Honestly, this article is the epitome of skin‑care enlightenment, darling-if you’re not using azelaic, you’re basically living in the dark ages of dermatology, lol.
Nis Hansen
November 30, 2025 AT 01:49
Reflect on the journey: every sunrise brings an opportunity to renew your skin’s narrative, and consistency is the philosopher’s stone that transforms pigment and pores alike.
Fabian Märkl
December 10, 2025 AT 15:32
Great rundown! 😊 Keep that sunscreen on point and let’s glow together! 🌞
Avril Harrison
December 21, 2025 AT 05:15
Nice overview, especially the bit about wearing hats-simple stuff that makes a big difference.
Natala Storczyk
December 31, 2025 AT 18:58
THIS IS A CALL TO ARMS!!! WE MUST DEFEND OUR SKIN FROM THE TYRANNY OF SUN AND HORMONES-NO MERCY!!!
nitish sharma
January 11, 2026 AT 08:41
Indeed, the protective measures you outlined are commendable; adherence to sunscreen and a balanced diet will fortify the epidermal barrier.
Rohit Sridhar
January 21, 2026 AT 22:24
Building on that, I would suggest monitoring glycemic load meticulously; studies show a correlation between insulin spikes and sebum production, which can exacerbate both melasma and acne. Moreover, consider integrating a low‑dose oral tranexamic regimen only under professional supervision, as it may synergize with topical azelaic to fade hyperpigmentation more rapidly.
Brian Van Horne
February 1, 2026 AT 12:06
Concise summary: cleanse, protect, treat, repeat; the fundamentals remain unchanged.
Norman Adams
February 12, 2026 AT 01:49
Oh, brilliant-because we all have time to read a novel about moisturizers while juggling life, right?