Every year, over 150,000 people in the U.S. end up in the emergency room because of something they ate with their medicine. It’s not rare. It’s not unusual. It’s happening to people who take pills daily-people like your neighbor, your parent, maybe even you. The problem isn’t the medicine. It’s not the food. It’s the gap between what’s written on the label and what’s actually happening at the dinner table.
You might not think about how your morning orange juice affects your blood pressure pill. Or how a handful of spinach could make your blood thinner stop working. Or how a glass of grapefruit juice can turn a safe dose of statin into a dangerous overdose. These aren’t myths. They’re documented, life-threatening interactions. And the easiest way to stop them? A simple, handwritten checklist you keep on your fridge.
Why Your Medication List Isn’t Enough
Most people keep a list of their meds. That’s good. But a list that just says “warfarin 5mg” or “simvastatin 20mg” doesn’t tell the full story. Medications don’t live in a vacuum. They react with what you eat, drink, and even supplement. The FDA says 12% of all drug-related ER visits involve food or drink. That’s one in eight. And it’s preventable.
A basic medication list tells your doctor what you take. A food-medication interaction checklist tells them what you shouldn’t take together. It’s the difference between knowing you have a gun and knowing where the safety is.
Take warfarin, for example. It’s a blood thinner. If you suddenly eat a big bowl of kale or spinach, your INR can drop. That means your blood clots faster. You’re at risk for stroke. But if you eat the same amount every day, your doctor can adjust your dose. That’s the key: consistency, not avoidance. Your checklist should say: “Warfarin - high risk with large changes in vitamin K foods (kale, spinach, broccoli). Keep daily intake steady. Do not skip or double up.”
What Goes on the Checklist
Start with your medications. Gather every pill, patch, liquid, or supplement. Keep them in their original bottles. Don’t guess. Look at the label. Write down:
- Brand name and generic name (e.g., Lipitor / atorvastatin)
- Dosage and frequency (e.g., 10mg once daily at bedtime)
- Why you take it (e.g., “lowers cholesterol”)
- Who prescribed it (e.g., Dr. Chen, Cardiology Associates)
- Phone number of the prescribing clinic
Now, for each one, list the food or drink interactions. Don’t rely on memory. Use trusted sources: the New Zealand Formulary, FDA Drug Safety Communications, or the SEFH Drug-Food/Herb Interaction Guide (2024 edition). Here’s what to include for each interaction:
- Food or drink: “Grapefruit juice,” “dairy products,” “aged cheese,” “red wine”
- Risk level: High, Moderate, Low
- Why it matters: “Grapefruit juice blocks enzyme that breaks down simvastatin - levels can spike 300-500%.”
- What to do: “Avoid completely,” “Wait 4 hours after taking pill,” “Limit to 1 small glass per day”
- Source: “FDA Drug Safety Communication #2023-045,” “NZ Formulary, July 2024”
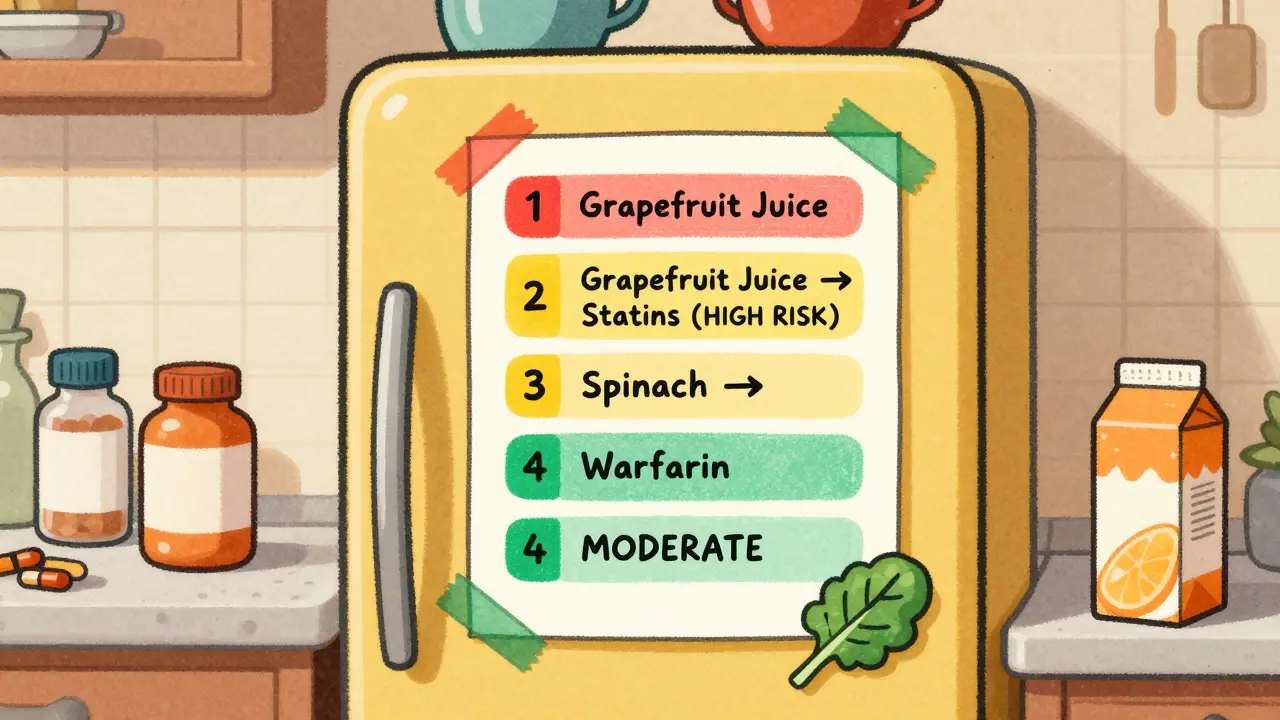
Some high-risk interactions you can’t ignore:
- Warfarin + vitamin K-rich foods: Don’t avoid them. Eat the same amount every day. A cup of cooked spinach has 1,000 mcg of vitamin K. A cup of raw has 145. Your checklist should note preparation method.
- Statins + grapefruit juice: Even one glass can cause muscle damage or kidney failure. Avoid completely.
- Ciprofloxacin + dairy: Calcium in milk, yogurt, or cheese blocks absorption. Take antibiotics 2 hours before or after dairy.
- MAO inhibitors + tyramine-rich foods: This includes aged cheese, cured meats, tap beer, soy sauce. Can cause dangerous spikes in blood pressure - up to 180/110.
- Linezolid + tyramine: Same risk as MAOIs. Even a small amount of blue cheese can trigger a hypertensive crisis.
High-Risk vs. Low-Risk: How to Rate It
Not all interactions are equal. Use this simple guide:
- High Risk: Can cause hospitalization, organ damage, or death. Requires complete avoidance or strict timing. Examples: grapefruit + statins, tyramine + MAOIs.
- Moderate Risk: Reduces effectiveness or causes mild side effects. Can be managed with timing. Examples: dairy + antibiotics, leafy greens + warfarin (if intake varies).
- Low Risk: Minimal or no known effect. Monitor if unsure. Examples: coffee + most SSRIs, chocolate + most blood pressure meds.
Color-code it. Use red for high, yellow for moderate, green for low. Stick it on your fridge with magnets. Make it impossible to miss.

Paper vs. Digital: Which One Works
You don’t need an app. In fact, many older adults do better with paper. A 2023 JAMA study found digital tools cut errors by 42% - but only 63% of people over 75 used them. Paper? 92% adoption.
Here’s the truth: paper wins for emergencies. If you fall, if you’re rushed to the ER, if your phone dies - a laminated checklist on your fridge saves lives. Digital tools update automatically. But they can be wrong. A 2024 FDA report found 62% of unregulated health apps gave inaccurate food-drug interaction info.
Best approach? Use both. Keep a paper checklist on your fridge. Use a trusted app like Medisafe or MyTherapy to track doses and get reminders. But don’t rely on the app for interaction warnings unless it’s FDA-recognized or linked to the New Zealand Formulary.
The FDA’s free “My Medicines” template (fda.gov/MyMedicines) is still the gold standard for paper. It has 12 fields per medication. Print it. Fill it out. Laminate it. Put it on the fridge.
How to Start - Step by Step
Don’t try to do it all at once. Set aside 45 minutes. Here’s how:
- Gather everything. Pull out every pill bottle, supplement jar, and OTC box. Include vitamins, herbal teas, and CBD oil.
- Write down each medication. Use the FDA’s 12-point format. Don’t skip anything.
- Look up each one. Go to the New Zealand Formulary interaction checker. Or search “FDA [drug name] food interaction.” Read the official medication guide.
- Rate the risk. High, moderate, or low. Write the action needed.
- Include allergies. Not just drugs - food allergies too. “Allergic to peanuts - anaphylaxis.”
- Add emergency contacts. Two people. Their names. Their numbers. Your pharmacist’s number.
- Write the date. “Last updated: January 15, 2026.” Update it every time your meds change.
Do this once. Then spend 5 minutes every Sunday checking it. Did you start a new pill? Update it. Did your doctor change your dose? Update it. Did you eat something new? Check if it’s on the list.
What to Do When You’re Not Sure
When in doubt, call your pharmacist. Not your doctor. Not Google. Your pharmacist. They’re trained for this. Every prescription you pick up? Ask: “Is there anything I shouldn’t eat or drink with this?”
Medicare Advantage plans now cover Medication Therapy Management (MTM) sessions. That’s a free 30-minute phone or in-person visit with a pharmacist who reviews your whole list - including food interactions. Call your plan. Ask if you qualify.
And if you’re on warfarin? Get your INR checked regularly. Your checklist helps your doctor know if your diet changed - not your dose.
Real Stories, Real Results
One Reddit user, on r/Pharmacy, shared how their checklist saved them. They were on tacrolimus after a kidney transplant. They drank grapefruit juice every morning. Their app didn’t warn them. Their checklist did. They stopped. Their kidney function stabilized. No hospital visit.
Another woman in Ohio had been on lisinopril for years. She loved her daily smoothie - spinach, banana, almond milk. Her doctor never asked about diet. Her checklist said: “Spinach - moderate risk with ACE inhibitors. May increase potassium.” She switched to kale. Her potassium levels normalized.
These aren’t rare. They’re common. And they’re preventable.
What Happens If You Don’t Do This
Without a checklist, you’re guessing. And guessing with medication is dangerous.
A 2023 FDA analysis found that 28% of checklist-related errors happened because people didn’t update their lists after a medication change. That’s not carelessness. That’s lack of system.
Worse, 43% of non-English speakers can’t understand warning labels. That’s why the American Heart Association is releasing free checklist templates in 15 languages by December 2024. If you or a loved one speaks another language - request one. It’s free.
And here’s the kicker: preventing one serious food-drug interaction saves the healthcare system $1,200 per person per year. That’s not just money. It’s a hospital bed. A doctor’s time. A family’s peace of mind.
You don’t need to be a doctor. You don’t need to be tech-savvy. You just need to write it down. And keep it visible.
Robin Van Emous
January 27, 2026 AT 00:11
Man, I never thought about how my grapefruit juice could mess with my statin. I’ve been drinking it every morning for years. Guess I’m switching to apple juice now. Thanks for the wake-up call.
Joanna Domżalska
January 28, 2026 AT 12:08
So let me get this straight-you’re telling me the solution to a complex medical system failure is a sticky note on the fridge? That’s like putting duct tape on a leaking nuclear reactor and calling it a fix.
Sally Dalton
January 29, 2026 AT 06:47
OMG YES THIS!! I just started warfarin last month and my grandma gave me this exact checklist and i cried because it felt so human?? i wrote it in crayon on a post-it and stuck it next to my coffee maker 🥹 i check it every morning like a ritual now. thank you for writing this.
Curtis Younker
January 29, 2026 AT 13:31
Look, I used to think this was overkill-until my uncle ended up in the ICU because he ate a whole wheel of blue cheese with his MAOI. I’m not even kidding. He thought ‘it’s just cheese.’ Now my whole family has laminated fridge checklists. We even have a color-coded magnet set. My 82-year-old mom updates hers every Sunday with her pill organizer. It’s not fancy, but it’s alive. And that’s what matters. If you’re reading this and you’re on more than three meds? Stop scrolling. Go grab your bottles. Write it down. Do it for the person you love who might not be able to speak up for themselves.
Shawn Raja
January 31, 2026 AT 06:07
Wow. So we’ve turned healthcare into a grocery list. Next they’ll ask us to rate our blood pressure meds by spice level. ‘Medium heat: avoid dairy. Extra spicy: don’t breathe near a grapefruit.’ At this point, I’m just waiting for the TikTok trend: #ChecklistChallenge. First you get the list, then you cry, then you post it with a #blessed hashtag. We’ve become a society that needs a sticky note to not die.
Allie Lehto
February 1, 2026 AT 02:55
This is why America is dying. People don’t read labels. They don’t ask questions. They just eat their grapefruit juice like it’s a right. And now you’re giving them a checklist like it’s a magic spell? No. The real problem is that we’ve outsourced our health to corporations and then act surprised when it backfires. Wake up. This isn’t about paper. It’s about accountability. And nobody wants to be accountable.
Henry Jenkins
February 1, 2026 AT 12:52
I’ve been using a digital app for my meds for two years, but I never realized how unreliable it was until I found a 2024 FDA report saying 62% of health apps give wrong interaction info. That’s insane. I switched to the FDA’s printable template after reading this. I printed two copies-one for the fridge, one for my wallet. I even added my pharmacist’s direct line. It took 45 minutes. Best 45 minutes I’ve spent in years. I feel like I finally have control. Also, I didn’t know about MTM sessions through Medicare Advantage. I’m calling my plan tomorrow.
Dan Nichols
February 2, 2026 AT 09:01
Why are you telling people to use the New Zealand Formulary? It’s not even American. The FDA has its own database. You’re overcomplicating this. Just use the pill bottle. It says ‘avoid grapefruit.’ Done. Also stop using ‘you’ like it’s a personal attack. It’s not a sermon.
Renia Pyles
February 4, 2026 AT 06:02
So let me guess-you’re the kind of person who also tells people to ‘just drink more water’ and ‘exercise more’ to fix chronic illness? This checklist is a band-aid on a severed artery. The real issue is pharmaceutical companies hiding interactions and doctors not having time to explain them. Stop blaming the patient. This isn’t a DIY project. It’s systemic failure dressed up as a productivity hack.
Rakesh Kakkad
February 4, 2026 AT 22:40
Dear friend, this is an excellent initiative. In India, we do not have such awareness. My father took losartan with potassium-rich banana daily. He suffered hyperkalemia. Now we print checklist in Hindi and English. We keep it near tea kettle. Thank you for your wisdom. I will share this with my village clinic.
Nicholas Miter
February 6, 2026 AT 21:05
I used to think this was too much work. Then I saw my mom forget her meds and eat a whole block of cheddar with her antibiotics. She got sick for a week. I made her a checklist. She calls it her ‘medicine buddy.’ Now she puts it next to her toothbrush. I didn’t even have to nag her. It just… worked. Sometimes the simplest things are the ones we ignore the most.
Suresh Kumar Govindan
February 8, 2026 AT 01:20
This is a placebo for the uneducated. The real solution is universal healthcare and mandatory pharmacist counseling. A fridge note does not fix corporate negligence. Also, grapefruit juice is not the enemy. The FDA is.
TONY ADAMS
February 9, 2026 AT 19:55
My cousin took simvastatin and drank grapefruit juice. He got rhabdo. Lost 40% muscle mass. Now he’s on a walker. I made him a checklist. He still drinks it. Says he’s ‘too old to change.’