When you're on warfarin, even a simple antibiotic can throw your blood-thinning levels out of balance - and that’s not just a minor concern. A spike in INR can mean life-threatening bleeding. For millions of people taking warfarin for atrial fibrillation, deep vein thrombosis, or mechanical heart valves, this isn’t theoretical. It’s a real, daily risk - and antibiotics are one of the most common triggers.
Warfarin works by blocking vitamin K, which your body needs to make clotting factors. But vitamin K doesn’t just come from your spinach. About 10-15% of it is made by bacteria in your gut. When you take certain antibiotics, you kill off those bacteria. That cuts your vitamin K supply. Less vitamin K means warfarin works too well. Your INR climbs. And when INR goes above 4.0, your risk of major bleeding jumps 4 to 8 times.
Why Some Antibiotics Are Much Riskier Than Others
Not all antibiotics affect warfarin the same way. The danger comes from two different mechanisms - and knowing which one is at play changes how you manage it.
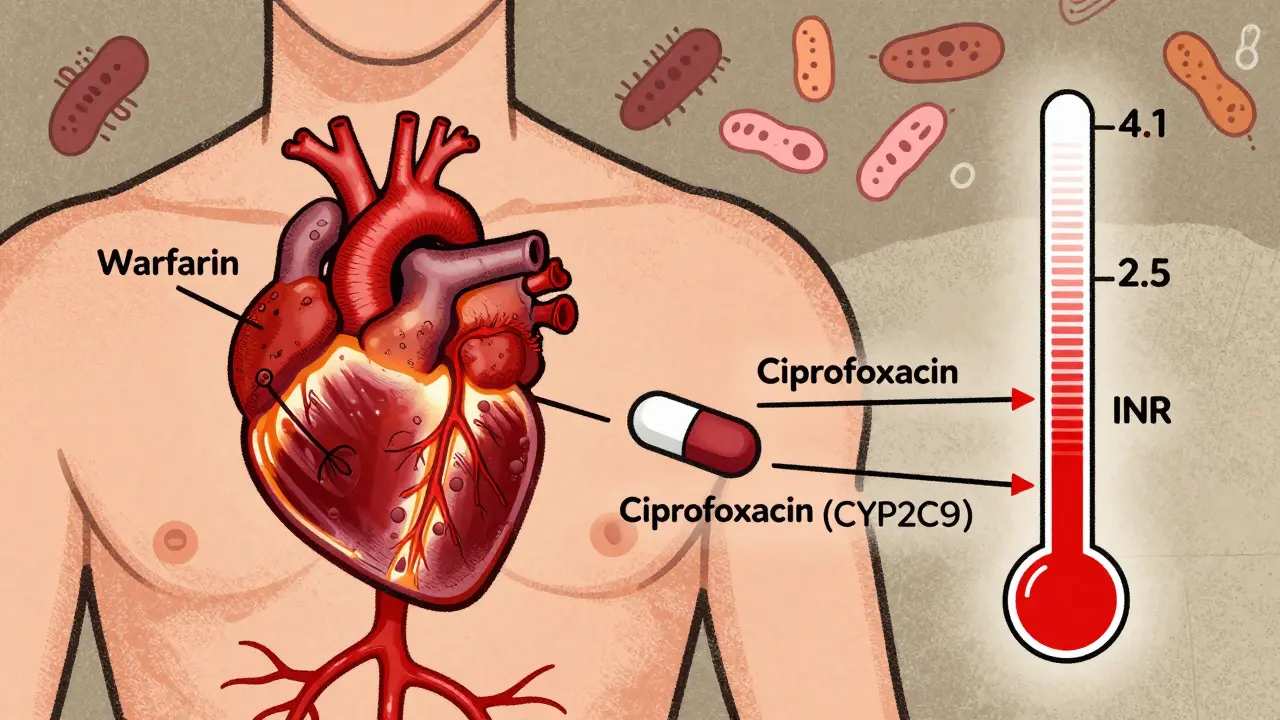
The first is enzyme interference. Warfarin is broken down in the liver by enzymes called CYP2C9, CYP1A2, and CYP3A4. Some antibiotics block these enzymes, causing warfarin to build up in your blood. Fluoroquinolones like ciprofloxacin and levofloxacin are big offenders. Studies show ciprofloxacin can push INR from 2.5 to 4.1 in just a week. Macrolides like erythromycin do the same. Even Bactrim (sulfamethoxazole/trimethoprim) is known to spike INR by an average of 1.8 units within five days.
The second mechanism is gut flora disruption. Antibiotics that wipe out vitamin K-producing bacteria - even if they don’t touch liver enzymes - can still cause dangerous INR rises. This includes amoxicillin/clavulanate and certain cephalosporins like cefotetan and cefoperazone. These drugs don’t inhibit CYP enzymes, but they still increase bleeding risk by 1.9-fold according to a 2024 review. That’s because they clear out the gut bugs that make your vitamin K.
On the flip side, some antibiotics are low-risk. Nitrofurantoin and fosfomycin don’t interfere with warfarin at all. Azithromycin (a macrolide) has minimal effect because it barely touches CYP enzymes. Ceftriaxone causes almost no INR change. And rifampin? It’s the opposite problem - it speeds up warfarin breakdown, dropping your INR and putting you at risk for clots.
When the INR Spike Hits - And How to Stop It
Timing matters. If an antibiotic blocks liver enzymes (like ciprofloxacin), your INR can jump within 48 to 72 hours. But if it’s killing gut bacteria (like amoxicillin), the spike usually hits 5 to 7 days after you start the antibiotic - and it can linger for up to 10 days after you stop.
That’s why checking your INR only once at the start isn’t enough. The American College of Chest Physicians recommends testing within 72 hours of starting the antibiotic, then twice a week until you finish. And don’t forget: you still need monitoring for a week after you stop the antibiotic. Bleeding risk peaks between days 8 and 14 - not when you’re still taking it.
Here’s what experts do in practice:
- For high-risk antibiotics (ciprofloxacin, erythromycin, Bactrim): Reduce your warfarin dose by 20-30% when you start the antibiotic. Check INR every 2-3 days. If INR rises above 4.0, hold your next dose and get medical help immediately.
- For gut flora disruptors (amoxicillin/clavulanate, cefotetan): No upfront dose change. Just check INR weekly. Only adjust warfarin if your INR goes above target range.
- For rifampin: Increase your warfarin dose by 50% right away. Monitor daily until stable. This isn’t optional - your INR will crash without it.
Real-world data from GoodRx shows that 42% of warfarin-related ER visits involve antibiotics. And ciprofloxacin, Bactrim, and amoxicillin/clavulanate account for 68% of those cases. That’s not random. It’s predictable - if you’re watching.

What You Should Do Right Now
If you’re on warfarin and your doctor prescribes an antibiotic, ask these three questions:
- Is this antibiotic known to interact with warfarin?
- Will you check my INR before I start, during, and after the course?
- What symptoms should I watch for - and when should I call?
Bleeding signs aren’t always dramatic. You might notice:
- Bruising without injury
- Bleeding gums when brushing
- Prolonged bleeding from a cut
- Dark, tarry stools or blood in urine
- Headaches, dizziness, or sudden weakness (could mean internal bleeding)
Don’t wait for a nosebleed to be serious. If you see any of these, contact your anticoagulation clinic or go to urgent care. Time is critical.
Pharmacists Are Your Secret Weapon
Most people think their doctor handles everything. But pharmacists - especially those in anticoagulation clinics - are the frontline in preventing these interactions. Studies show that when pharmacists manage warfarin during antibiotic use, bleeding complications drop by 37%. Why? Because they catch the risks doctors miss. They know which antibiotics are dangerous. They track INR trends. They adjust doses proactively.
If you’re on warfarin, find out if your pharmacy offers a warfarin monitoring service. Many do - and it’s often free with insurance. Don’t wait until you’re in the ER to use it.
What’s Changing in 2026
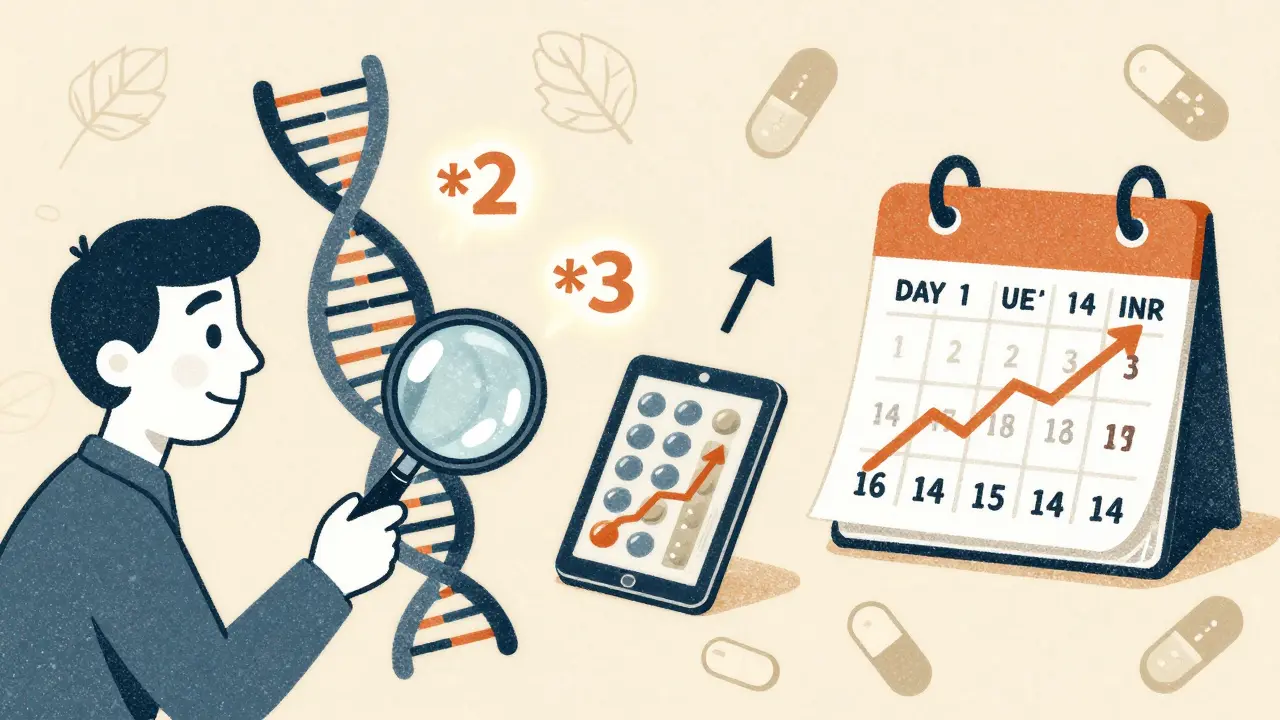
Science is moving beyond guesswork. A 2022 study found that people with certain CYP2C9 gene variants (*2 or *3) have 2.4 times greater INR spikes when taking antibiotics. That means your genetics could tell you how risky a certain antibiotic will be for you.
The 2023 WARF-GEN trial showed that using genetic testing to guide warfarin dosing during antibiotic therapy reduced INR instability by 41%. That’s huge. It means in the near future, your doctor might test your DNA before prescribing an antibiotic - not just to avoid bleeding, but to personalize your care.
Meanwhile, newer antibiotics like tetizolid are showing minimal interaction. That’s good news. But until everyone’s on genetic testing, we still have to treat every antibiotic as a potential threat.
Bottom Line: Don’t Assume It’s Safe
There’s no such thing as a "safe" antibiotic for warfarin users - only "lower risk." Even if your doctor says "it’s fine," ask for an INR check. Don’t rely on memory or old advice. The rules changed. The data is clear. And the consequences are too serious to gamble with.
Keep a log of your INR values. Write down every antibiotic you take - even over-the-counter ones. Tell every new doctor you’re on warfarin. And if you’re unsure? Call your anticoagulation clinic. Better safe than bleeding.
Can I take amoxicillin while on warfarin?
Yes, but with caution. Amoxicillin/clavulanate (Augmentin) can lower vitamin K production in your gut, leading to INR spikes. You don’t need to stop it, but you should have your INR checked before starting, again 5-7 days later, and again after finishing the course. No dose change is needed upfront unless your INR rises above your target range.
Which antibiotics are safest with warfarin?
Nitrofurantoin and fosfomycin show no significant interaction with warfarin. Azithromycin is also low-risk because it doesn’t inhibit liver enzymes. Ceftriaxone causes minimal INR changes. But even these require monitoring - no antibiotic is completely risk-free in warfarin users.
How long does it take for INR to return to normal after an antibiotic?
It depends on the mechanism. If the antibiotic blocked liver enzymes (like ciprofloxacin), INR usually normalizes within 72 hours of stopping. If it killed gut bacteria (like amoxicillin), it can take 7-10 days - sometimes longer - for your vitamin K levels to recover. Always monitor INR for at least a week after finishing the antibiotic.
What if my INR is 5.0 or higher?
If your INR is 5.0 or above and you have no bleeding symptoms, your provider may skip your next warfarin dose and give you a small amount of oral vitamin K. If your INR is over 8.0, or if you’re bleeding, you’ll need urgent medical care - possibly IV vitamin K, fresh frozen plasma, or hospitalization. Never ignore a high INR.
Should I avoid antibiotics altogether if I’m on warfarin?
No. Infections can be life-threatening, and untreated infections raise your risk of clotting more than antibiotics raise your bleeding risk. The goal isn’t to avoid antibiotics - it’s to manage them carefully. With proper monitoring, most people on warfarin can safely take antibiotics without complications.
Tom Forwood
February 10, 2026 AT 02:36
Man I wish I knew this before I took cipro for that UTI last year. My INR shot to 5.2 and I ended up in the ER with a black eye from a nosebleed that wouldn’t stop. Docs just shrugged and said "oh weird". Turns out they didn’t even check my INR before prescribing. Don’t let this happen to you. Always ask. Always check. Always write it down.
John Sonnenberg
February 10, 2026 AT 13:44
Let me be crystal clear: antibiotics are not harmless. They are not "fine." They are silent killers in disguise. If your doctor prescribes you something without checking your INR first, they are not your friend. They are a liability. And if you’re not monitoring your INR for a full week after finishing, you’re gambling with your life. No ifs, ands, or buts.
Joshua Smith
February 12, 2026 AT 01:09
This is such a helpful breakdown. I’ve been on warfarin for 8 years and never realized how much gut health plays into it. I always thought it was just liver enzymes. Learning that amoxicillin/clavulanate messes with vitamin K production explains why my INR spiked last time even though I wasn’t on a "high-risk" drug. Thanks for clarifying the timeline too-7-10 days after stopping is way longer than I expected.
Jessica Klaar
February 13, 2026 AT 21:19
I’m so glad someone wrote this. My mom had a scary episode last winter after taking Bactrim for a sinus infection. She didn’t tell her doctor she was on warfarin because she thought it was "just a cold." We ended up in the hospital at 3 a.m. with a hematoma the size of a grapefruit. This post saved me from panicking-I now have a printed list of safe vs risky antibiotics taped to the fridge. Everyone on warfarin should save this. Seriously.
PAUL MCQUEEN
February 15, 2026 AT 08:59
Okay, but why are we still using warfarin at all? There are so many newer anticoagulants that don’t have these stupid interactions. Why are we still putting people through this? It’s 2024. Why are we still playing Russian roulette with antibiotics? Someone needs to update the guidelines already.
glenn mendoza
February 16, 2026 AT 14:43
Thank you for this meticulously researched and deeply compassionate overview. The clinical implications of this information cannot be overstated. I have witnessed firsthand the tragic consequences of underestimating these interactions. The recommendation to monitor INR for a full week post-antibiotic course is not merely prudent-it is lifesaving. I urge all healthcare providers to institutionalize this protocol. The data speaks clearly. The time for complacency has passed.
THANGAVEL PARASAKTHI
February 16, 2026 AT 17:56
Bro this is gold. I’m from India and my doc here didn’t even know about cefotetan being risky. I showed him this and he was like "huh, never saw that." Now he’s sending me for INR checks every 3 days. Also, azithromycin is my new BFF. No more cipro for me. And yeah, pharmacists are the real MVPs. My local one remembers my INR history like it’s my birthday.
Chelsea Deflyss
February 17, 2026 AT 01:45
Ugh I hate when people make this sound like a big mystery. It’s just basic pharmacology. If you’re on warfarin and take an antibiotic, your INR goes up. Duh. Stop acting like this is new. Also, why is everyone so obsessed with amoxicillin? I’ve taken it 5 times and never had an issue. Probably just lucky.