When your kidneys stop working, your body doesn’t just slow down-it starts to drown in its own waste. Uremic symptoms aren’t just discomforts; they’re warning signs that your body is reaching a breaking point. Nausea, itching, and fatigue aren’t normal aging. They’re signals that toxins are building up in your blood because your kidneys can’t filter them out anymore. If you’re living with advanced kidney disease, understanding these symptoms and knowing when dialysis becomes necessary can mean the difference between barely getting by and actually feeling like yourself again.
What Exactly Is Uremia?
Uremia isn’t a disease-it’s the result of kidney failure. When your kidneys drop below 10-15% of normal function, they can’t remove urea, creatinine, and other metabolic waste products. These toxins pile up in your bloodstream, and your body reacts. It’s not just about high numbers on a lab report; it’s about how you feel. A BUN (blood urea nitrogen) level above 80 mg/dL and a creatinine level over 8 mg/dL are common thresholds where symptoms start to become unavoidable. But numbers alone don’t tell the whole story. Two people with the same lab values can feel completely different. That’s why symptoms matter more than numbers when deciding to start dialysis.
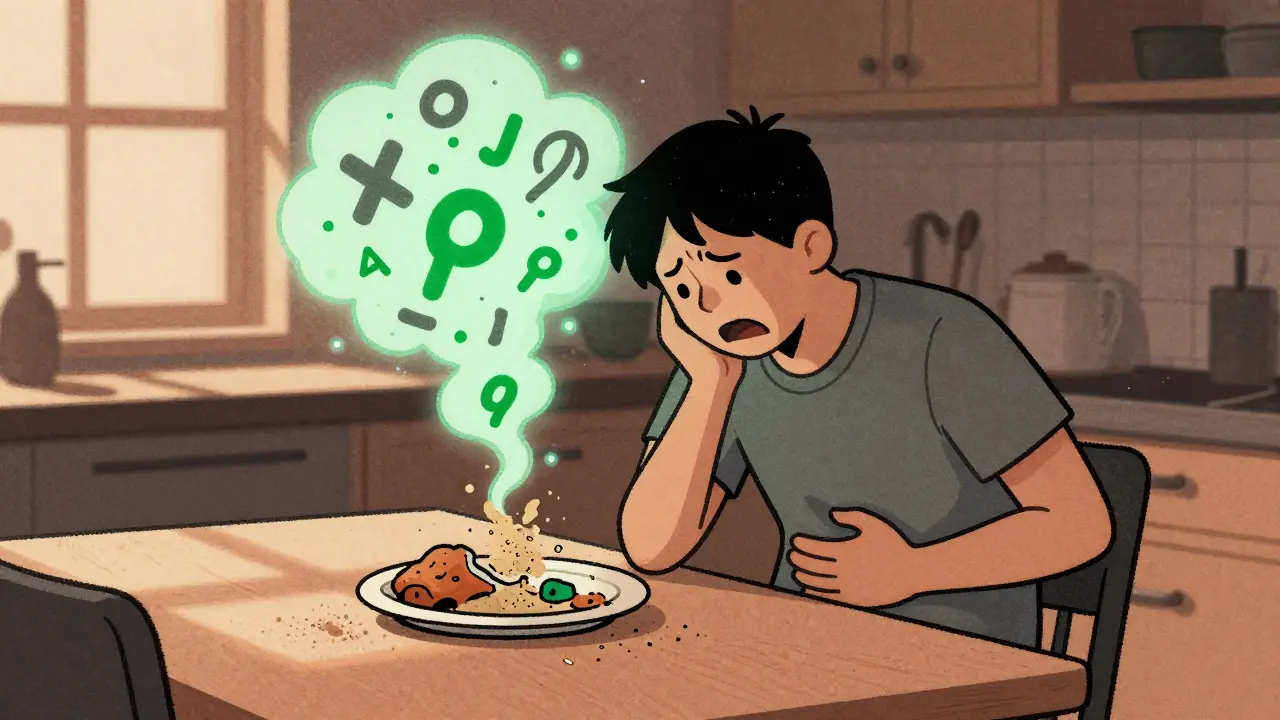
Nausea: When Food Becomes a Chore
Imagine waking up and feeling sick just from the smell of coffee. Or eating a meal and immediately regretting it. For many people with advanced kidney disease, nausea isn’t occasional-it’s constant. Studies show that about 68% of patients in stage 5 chronic kidney disease (CKD) experience nausea regularly. It’s not just stomach upset. It’s tied to specific toxins like p-cresyl sulfate and indoxyl sulfate, which build up when kidneys fail. These chemicals trigger the brain’s vomiting center, even when there’s nothing wrong with your stomach.
One patient described it as "eating sand"-a metallic, gritty taste that made even favorite foods unbearable. Weight loss follows fast. In one study, patients lost an average of 5% of their body weight over three months because they couldn’t keep food down. That’s not just inconvenience; it’s malnutrition that weakens your immune system and makes recovery from any illness harder. Ondansetron (Zofran) is often the first treatment tried, but it doesn’t work for everyone. Domperidone helps some, but it carries heart risks, especially with kidney disease. The real fix? Dialysis. Once it starts, nausea usually improves within days.
Itching: The Sleep-Stealing Symptom
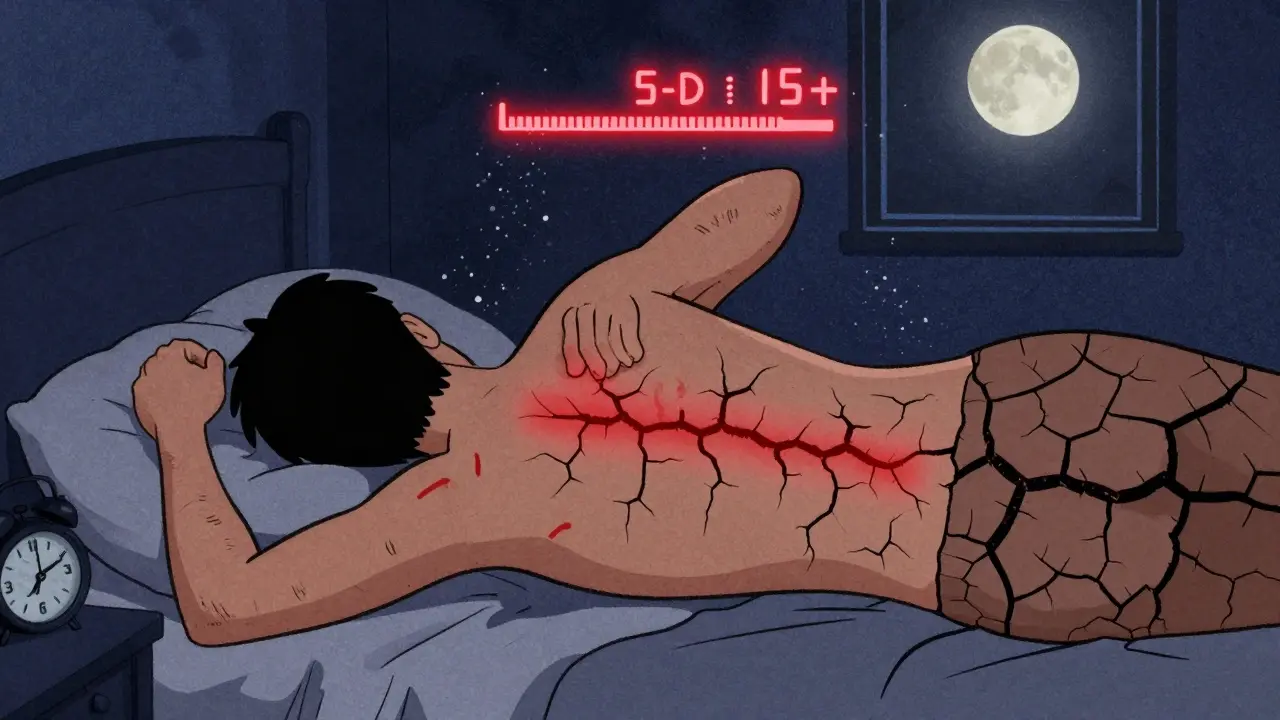
If you’ve ever had dry skin from winter, imagine that-but worse, all over, day and night, and nothing helps. This is uremic pruritus, or CKD-associated pruritus. It affects up to 70% of people on hemodialysis and still hits nearly 40% of those not yet on dialysis. It’s not caused by dry skin. It’s caused by inflammation, nerve changes, and toxins like phosphate and parathyroid hormone that build up in the blood.
Most people feel it on their back, arms, and legs-not just one spot. It’s symmetrical, meaning both sides of the body itch the same. And it gets worse at night. One Reddit user, "DialysisDad," said he scratched until he bled. His Fitbit sleep score dropped from 85 to 42 over six months. That’s not exaggeration-it’s documented. Studies show patients with severe itching have CRP levels (a marker of inflammation) more than double those without itching.
Doctors use the 5-D Itch Scale to measure severity: Duration, Degree, Direction, Disability, and Distribution. A score over 12 means it’s severe. Over 15? That’s a red flag. Many patients change jobs, avoid social events, or stop sleeping because of it. The good news? Treatments exist. Gabapentin helps some. Difelikefalin (Korsuva), approved by the FDA in 2021, reduces itching by over 30% in weeks. Nalfurafine, a newer drug, works even faster. But none of these work as well as dialysis itself.
When Should Dialysis Start? The Real Answer
For decades, doctors waited until patients were barely conscious before starting dialysis. That’s changed. The 2023 KDOQI guidelines say: don’t wait for collapse. But you also shouldn’t start too early. The IDEAL trial, a major 2020 study, found no survival benefit to starting dialysis at eGFR 10-14 versus 5-7. So why wait? Because symptoms are the true trigger.
Here’s what experts agree on:
- Start dialysis when symptoms like nausea, itching, or fatigue interfere with daily life-not just because your eGFR is 9.
- If you’ve lost 5% of your body weight in 3 months because you can’t eat, dialysis is likely needed.
- If itching is keeping you awake every night and scoring over 15 on the 5-D scale, it’s time.
- If you have signs of uremic pericarditis (chest pain, fluid around the heart), dialysis is urgent.
Some doctors still push for earlier dialysis to "prevent" complications. But the data doesn’t support it. A 2021 Japanese study showed fewer hospitalizations with early dialysis, but those patients were younger and healthier overall. For most, the goal isn’t to start early-it’s to start when you need it. Waiting too long can be dangerous. Starting too soon doesn’t extend life-it just adds time on a machine.
What Happens If You Wait Too Long?
Delaying dialysis when symptoms are clear can lead to serious, avoidable problems. Fluid overload can cause heart failure. High potassium can trigger dangerous heart rhythms. Severe itching can lead to skin infections from constant scratching. Nausea and vomiting can cause dehydration and electrolyte imbalances. One study found patients who delayed dialysis past symptom onset had a 58% higher risk of death in the first year compared to those who started when symptoms appeared.
And it’s not just physical. The mental toll is heavy. Patients report depression, anxiety, and social isolation. One survey found 28% changed careers because they couldn’t work with constant nausea or itching. Another found 41% visited three or more doctors before getting the right diagnosis. That delay averages 8.7 months. That’s over half a year of suffering that could have been prevented.

What Can You Do Before Dialysis?
While you’re waiting for dialysis to start-or if you’re trying to delay it-there are steps to manage symptoms:
- For nausea: Eat small, bland meals. Avoid strong smells. Try ginger tea or peppermint. Avoid high-phosphate foods like dairy, processed meats, and soda.
- For itching: Use fragrance-free moisturizers. Take lukewarm baths with colloidal oatmeal. Avoid hot showers. Keep nails short. Ask your doctor about phosphate binders-these can reduce itching by lowering blood phosphate levels.
- For both: Work with a renal dietitian. Track your symptoms daily. Use a symptom journal. Note when nausea hits, how bad the itch is, and what made it worse. This helps your doctor decide when to act.
Phosphate binders like sevelamer or lanthanum can reduce itching and nausea by lowering toxin levels. But they’re not a cure. They just buy time. Dialysis remains the only way to remove these toxins effectively.
The Hidden Inequality
Not everyone gets care at the same time. A 2023 study found Black patients waited 3.2 months longer than White patients before starting dialysis, even with the same symptoms. That delay led to 18% more hospitalizations. Why? Access to specialists, distrust in the system, lack of education, and insurance barriers all play a role. If you’re struggling to get answers, ask for a nephrology social worker. They’re trained to help navigate these gaps.
What’s Next?
The future of dialysis decisions is shifting. New tools like the PROMIS-Itch scale are being tested to measure symptom severity more accurately. By 2025, guidelines may require a symptom score over 15-not just lab numbers-to trigger dialysis. That’s progress. It means your experience matters as much as your lab results.
For now, the message is clear: Don’t ignore nausea. Don’t brush off itching. These aren’t "just part of aging." They’re signs your kidneys are failing. And when they’re severe enough to ruin your sleep, your appetite, or your ability to work, it’s time to talk about dialysis-not tomorrow, not next month, but now.
Is uremic itching the same as regular dry skin?
No. Uremic itching (CKD-aP) isn’t caused by dry skin. It’s linked to toxins, inflammation, and nerve changes from kidney failure. It affects large areas of the body symmetrically, gets worse at night, and doesn’t respond to typical moisturizers or antihistamines. If you have persistent itching with advanced kidney disease, it’s likely uremic, not dry skin.
Can you manage uremic symptoms without dialysis?
You can manage symptoms temporarily with diet, medications, and phosphate binders, but you can’t reverse the underlying problem. Dialysis is the only treatment that removes the toxins causing nausea and itching. Medications like gabapentin or difelikefalin help reduce itching, and ondansetron helps with nausea-but they don’t fix the root cause. Without dialysis, symptoms will return and worsen.
How do I know if I’m ready for dialysis?
You’re likely ready if: (1) you’ve lost weight because you can’t eat, (2) itching keeps you awake every night, (3) nausea makes daily tasks impossible, or (4) your eGFR is below 10.5 and symptoms aren’t improving with treatment. Your nephrologist will look at your symptoms, lab results, and quality of life-not just one number.
Does starting dialysis early extend life?
Not necessarily. The IDEAL trial showed no survival benefit for starting dialysis at eGFR 10-14 versus 5-7. What matters more is symptom control. Starting too early can lead to unnecessary complications and lower quality of life. The goal is to start when symptoms become unmanageable-not just because your number dropped.
Why does dialysis help with itching and nausea?
Dialysis removes the toxins that build up when kidneys fail-especially urea, creatinine, p-cresyl sulfate, and indoxyl sulfate. These chemicals directly trigger nausea centers in the brain and cause inflammation that leads to itching. Once dialysis starts, these toxins are flushed out, and symptoms usually improve within days to weeks.
Chiruvella Pardha Krishna
February 15, 2026 AT 21:42
There's something deeply poetic about the body drowning in its own waste. We think of kidneys as filters, but they're more like silent guardians-until they don't guard anymore. Uremia isn't just medical; it's existential. The nausea, the itch-they're not symptoms. They're the body's last whispered protest before the silence.
And yet, we treat it like a technical glitch. Fix the numbers, swap the machine, move on. But what about the man who can't eat his daughter's birthday cake because it smells like metal? Or the woman who scratches her arms raw because sleep is a luxury she can't afford?
We reduce suffering to eGFR thresholds. That’s not medicine. That’s statistics wearing a white coat.
Erica Banatao Darilag
February 16, 2026 AT 05:21
I appreciate how thoroughly this was explained. I work in patient advocacy and see too many people dismissed because their labs aren't 'bad enough.' The idea that symptoms should drive the decision-not just numbers-is so important. I've had clients who waited months because their creatinine was 7.8 instead of 8.2. That kind of delay is cruel.
Also, the part about phosphate binders buying time but not fixing the root issue? Spot on. So many patients think they're 'managing' when they're just postponing the inevitable. We need better education.
Mandeep Singh
February 17, 2026 AT 00:27
Oh please. You're telling me we need to wait until someone is literally crying from itching and vomiting into a bucket before we act? That's not patient-centered care-that's negligence wrapped in a 'let them suffer first' philosophy.
The IDEAL trial? Please. It was full of middle-class white guys with good insurance and access to dietitians. What about the single mom in rural Alabama who can't get a nephrology appointment for six months? Or the guy in India who can't afford phosphate binders? You think dialysis is a choice? It's a lifeline-and we're making people beg for it.
And don't get me started on how Black patients wait longer. This isn't medicine. It's systemic racism with a stethoscope.
Start dialysis when symptoms appear. Not when the numbers are 'scary enough.' Your kidneys aren't a spreadsheet. They're life.
Betty Kirby
February 18, 2026 AT 13:17
Let me just say-this is the most accurate, gut-punching breakdown of uremia I’ve ever read. The way you described itching as symmetrical and sleep-stealing? That’s my aunt. She scratched her legs till they bled. No eczema. No allergies. Just pure, unrelenting uremic pruritus. No one believed her until her CRP hit 22.
And the part about weight loss? She lost 18 pounds in three months. No one noticed because she was ‘just not eating right.’
Thank you for naming the invisible. Now if only the medical system would listen.
Josiah Demara
February 19, 2026 AT 11:50
Look, I’m not here to coddle anyone. But if you’re waiting for symptoms to be ‘bad enough’ to start dialysis, you’re already too late. You think nausea is ‘inconvenient’? Try having your liver shut down because you’re dehydrated from vomiting while your potassium hits 6.8.
And don’t even get me started on the ‘early dialysis doesn’t help’ crowd. The Japanese study showed fewer hospitalizations. Fewer hospitalizations means less cost, less trauma, less death. You want to wait until someone’s in the ER with pericardial tamponade? Fine. But don’t pretend you’re being patient-centered. You’re being cheap.
Also, phosphate binders? They’re not ‘buying time.’ They’re delaying the inevitable while the toxins cook your nerves. That’s not treatment. That’s torture with a receipt.
Kaye Alcaraz
February 21, 2026 AT 05:01
You’ve given us a roadmap-not just of medical facts, but of human suffering. And that’s what matters. I’ve worked with dialysis patients for over a decade. The ones who started when symptoms hit? They lived longer. They slept better. They hugged their grandchildren again.
The ones who waited? They lost jobs. They lost dignity. They lost hope.
Let’s stop talking about numbers. Let’s start talking about lives.
Thank you for this.
Sarah Barrett
February 21, 2026 AT 12:05
The most chilling part? That 8.7-month diagnostic delay. That’s not just a statistic. That’s 263 days of someone thinking they’re going crazy. Of being told it’s stress. Of being told to drink more water. Of being told to ‘just eat better.’
And then, when they finally get to a nephrologist, they’re told, ‘You’re not quite there yet.’
That’s not medicine. That’s gaslighting with a stethoscope.
Charlotte Dacre
February 23, 2026 AT 00:32
So let me get this straight: we wait until someone is too weak to lift a spoon before we save them? Brilliant. Just brilliant. Next you’ll tell me we should wait until the patient starts floating away before we give them oxygen.
Of course, if you’re rich, you get dialysis at eGFR 12. If you’re poor? You get to wait until your skin cracks open and your heart starts acting up. Classic.
And the fact that this is still even a debate? I’m speechless. (Which, given my sarcasm, is saying something.)
Esha Pathak
February 24, 2026 AT 20:28
Uremia is the universe’s quietest scream. No one hears it because it doesn’t scream loud enough for a lab report. It whispers in the silence between meals. In the sleepless nights. In the way a mother stops hugging her kids because she doesn’t want them to smell her.
And yet-we measure it in milligrams per deciliter.
We have the technology to see the toxins. But we refuse to see the person.
Maybe the real kidney failure isn’t in the body.
Maybe it’s in our ethics.
Mike Hammer
February 26, 2026 AT 07:02
Man, I never thought about how itching could ruin your whole life. I had a buddy on dialysis who stopped going to family dinners because he’d scratch so hard he’d bleed. Said he’d rather be alone than have people stare.
And the weight loss thing? Dude lost 20 lbs in 3 months. Couldn’t even hold his coffee cup. We thought he was on drugs. Turns out, his kidneys were just done.
Thanks for putting this out there. People need to know this isn’t normal aging. It’s a medical emergency.
Daniel Dover
February 26, 2026 AT 12:34
Start dialysis when symptoms interfere with life. Simple. Clear. Human.
Joe Grushkin
February 27, 2026 AT 22:51
Oh wow. Another ‘listen to your body’ manifesto. How quaint. You think the body’s a oracle? It’s a biological machine with a faulty firmware update. You don’t wait for the engine to explode before you fix the oil pump. You fix it before it fails.
And your ‘symptom-based’ approach? That’s just a euphemism for ‘let them suffer until they’re useful enough to justify the cost.’
The data doesn’t support early dialysis? Fine. But the data also doesn’t account for quality of life. You think someone who can’t sleep for six months because of itching is ‘fine’? That’s not medicine. That’s economics in a lab coat.
Virginia Kimball
March 1, 2026 AT 22:37
This gave me chills. I’ve watched two family members go through this. The first one started dialysis too early-felt like a robot for two years. The second waited until she couldn’t stand up. She cried the first time she ate a real meal after her first session. Said it tasted like sunshine.
There’s no perfect timing. But there’s a right timing.
And it’s when the person stops feeling like themselves.
You’re not just treating kidneys. You’re restoring humanity.