Introduction to Besifloxacin
In recent years, besifloxacin has emerged as a promising solution in the management of post-operative ocular infections. As a copywriter, I find it essential to explore this topic and provide information on the role of besifloxacin in treating eye infections following surgery. In this article, we will discuss various aspects of besifloxacin, including its mechanism of action, efficacy, and safety profile.
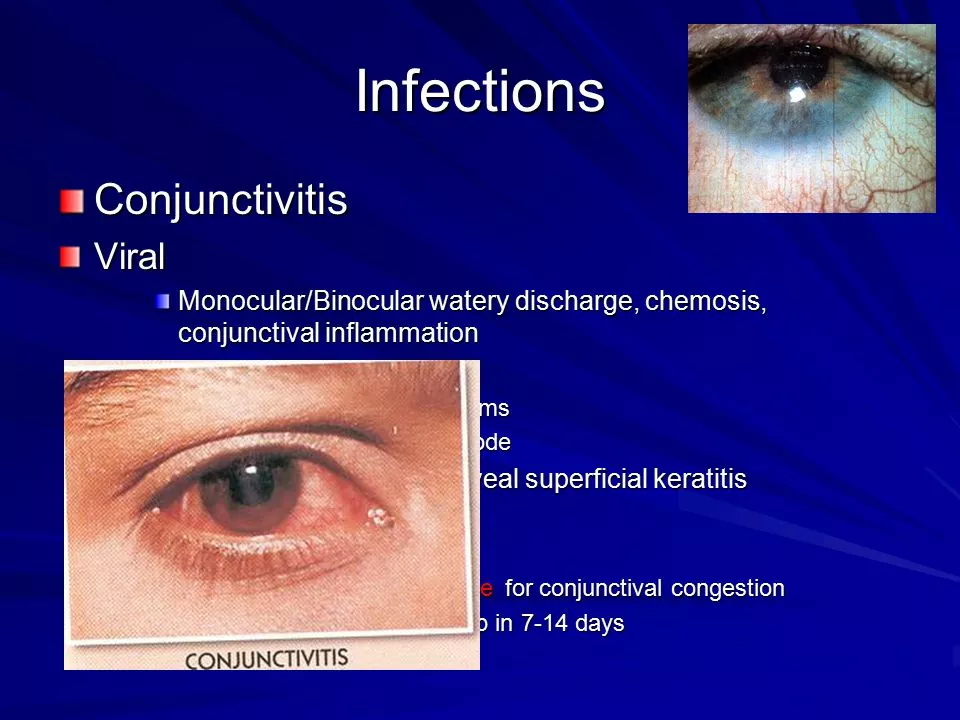
Understanding Post-operative Ocular Infections
Post-operative ocular infections are a common complication that can occur following eye surgery. These infections can lead to serious consequences, such as vision loss or even blindness, if not properly managed. The most common types of post-operative ocular infections include bacterial conjunctivitis, bacterial keratitis, and endophthalmitis. Treatment typically involves the use of topical antibiotics, but selecting the right antibiotic is crucial for ensuring a successful outcome.
Mechanism of Action of Besifloxacin
Besifloxacin is a fluoroquinolone antibiotic that has been specifically developed for the treatment of ocular infections. Its unique mechanism of action sets it apart from other antibiotics in its class. Besifloxacin works by inhibiting bacterial DNA gyrase and topoisomerase IV, two essential enzymes responsible for DNA replication, transcription, and repair in bacterial cells. This dual inhibition results in rapid bactericidal activity and helps to minimize the development of antibiotic resistance.
Efficacy of Besifloxacin in Treating Ocular Infections
Several clinical trials have demonstrated the efficacy of besifloxacin in treating post-operative ocular infections. These studies have shown that besifloxacin is highly effective against a wide range of bacteria, including both Gram-positive and Gram-negative organisms. In addition, besifloxacin has been found to be more potent than other fluoroquinolones, such as moxifloxacin and gatifloxacin, in treating ocular infections. This enhanced potency is believed to be due to its unique chemical structure and dual mechanism of action.
Safety Profile of Besifloxacin
One of the main concerns when using antibiotics is the potential for side effects and adverse reactions. Fortunately, besifloxacin has been shown to have a favorable safety profile in clinical trials. The most common side effects reported with besifloxacin use are mild and transient, such as eye irritation, redness, and itching. Serious side effects, such as corneal toxicity or systemic effects, have been reported rarely. This favorable safety profile makes besifloxacin an attractive option for treating post-operative ocular infections.
Resistance to Besifloxacin
Antibiotic resistance is a growing concern in the medical community, and it is essential to consider the potential for resistance when selecting an antibiotic for treatment. Besifloxacin has been shown to have a lower likelihood of developing resistance compared to other fluoroquinolones. This is likely due to its dual mechanism of action, which targets two essential bacterial enzymes. Additionally, besifloxacin has demonstrated activity against some fluoroquinolone-resistant strains, making it a valuable option in cases where resistance is a concern.
Dosing and Administration of Besifloxacin
Besifloxacin is available as a 0.6% ophthalmic suspension, which is typically administered as one drop in the affected eye(s) three times daily for five to seven days. The dosing schedule may be adjusted based on the severity of the infection and the patient's response to treatment. It is important to follow the prescribed dosing regimen to ensure the best possible outcome and minimize the risk of antibiotic resistance.
Comparing Besifloxacin with Other Antibiotics
When selecting an antibiotic for the treatment of post-operative ocular infections, it is essential to consider factors such as efficacy, safety, and resistance potential. Besifloxacin has demonstrated superior potency compared to other fluoroquinolones and has a favorable safety profile. Additionally, its dual mechanism of action and lower likelihood of developing resistance make it an attractive option for treating ocular infections. However, it is crucial to consider individual patient factors and consult with an eye care professional before selecting an antibiotic for treatment.
Conclusion
In conclusion, besifloxacin is a promising solution for the management of post-operative ocular infections. Its unique mechanism of action, potent bactericidal activity, and favorable safety profile make it an attractive option for eye care professionals and patients alike. As a copywriter, I hope that this article has provided valuable information on the role of besifloxacin in treating ocular infections following surgery and has contributed to a better understanding of its potential benefits.
Erin Leach
April 27, 2023 AT 06:24
I appreciate the thorough overview of besifloxacin-it really seems like a solid option for post‑operative eye infections. The safety profile you outlined gives both patients and clinicians confidence. It’s good to see a drug that balances potency with tolerability.
Erik Redli
May 6, 2023 AT 20:48
Honestly, the hype around besifloxacin is overblown. Sure, it hits a broad spectrum, but we’re still seeing resistance creep in, and the cost isn’t cheap. I’d rather stick with older, proven agents until the data is rock solid.
Jennyfer Collin
May 16, 2023 AT 11:12
One must consider the larger pharmaco‑industrial agenda when evaluating any novel ophthalmic agent. The rapid market approval of besifloxacin raises questions about the thoroughness of regulatory scrutiny. Moreover, the promotional literature often omits long‑term surveillance data, which could mask subtle adverse effects. It is prudent to remain skeptical of claims that a single drug can single‑handedly curb antibiotic resistance across diverse bacterial populations. While the dual‑target mechanism appears impressive, history teaches us that bacteria inevitably evolve clever work‑arounds. In addition, the concentration of marketing dollars may influence prescribing habits more than pure clinical merit. Thus, clinicians should weigh independent evidence over manufacturer narratives. 🧐
Tim Waghorn
May 26, 2023 AT 01:36
Besifloxacin’s pharmacodynamic profile merits a detailed examination, particularly in the context of postoperative ocular prophylaxis. The compound exhibits a dual inhibitory action on DNA gyrase and topoisomerase IV, which confers a rapid bactericidal effect against both Gram‑positive and Gram‑negative organisms. Clinical trials have demonstrated cure rates exceeding 90% for bacterial conjunctivitis and keratitis when administered thrice daily. Its 0.6% ophthalmic suspension ensures adequate corneal penetration while maintaining a favorable ocular surface tolerability. Adverse events reported are predominantly mild, such as transient burning or redness, with no significant systemic absorption observed. Resistance development appears limited, likely due to the simultaneous targeting of two essential bacterial enzymes, reducing the likelihood of single‑point mutations conferring survival advantage. Nevertheless, surveillance studies are essential to monitor for emerging resistance patterns, especially in settings with high fluoroquinolone usage. The dosing regimen of three drops per day for five to seven days aligns with standard postoperative protocols, facilitating patient adherence. Adjustments may be warranted in cases of severe infection or compromised ocular barriers, where intensified therapy could be beneficial. Comparative data suggest besifloxacin outperforms older fluoroquinolones like ciprofloxacin in vitro, though head‑to‑head clinical comparisons remain limited. From a safety perspective, the absence of corneal toxicity in multicenter studies supports its routine use. However, clinicians should remain vigilant for allergic reactions, particularly in patients with a history of hypersensitivity to quinolone derivatives. In practice, the decision to employ besifloxacin should be individualized, considering microbial culture results, patient comorbidities, and potential drug interactions. Overall, the current evidence positions besifloxacin as a valuable addition to the ophthalmic antimicrobial armamentarium, provided its use is guided by stewardship principles.
Brady Johnson
June 4, 2023 AT 16:00
While the data looks polished, the reality in clinic is far messier. I've seen patients develop inexplicable irritation that escalates into more serious inflammation, and the literature conveniently glosses over these outliers. Moreover, the aggressive marketing pushes us to prescribe a pricey drop when a simple generic would suffice. The drama surrounding "dual mechanisms" feels like a sales gimmick rather than a breakthrough.
Jay Campbell
June 14, 2023 AT 06:24
Good points all around. I think besifloxacin adds a useful tool, especially when cultures show resistant strains. It's helpful to have another option in our antibiotic toolbox.
Laura Hibbard
June 23, 2023 AT 20:48
Sure, another "miracle drop"-because what we really need is more hype and fewer real solutions. 🙄
Rachel Zack
July 3, 2023 AT 11:12
We must not forget the ethical responsibility of prescribing antibiotics wisely.
Lori Brown
July 13, 2023 AT 01:36
Absolutely agree! Let’s keep using besifloxacin responsibly-our patients will thank us. 😊
Jacqui Bryant
July 22, 2023 AT 16:00
Besifloxacin looks promising, and I hope it helps more patients recover quickly.
Paul Luxford
August 1, 2023 AT 06:24
Indeed, a hopeful addition to our treatment options. Proper use will be key.