COPD Risk Calculator
Your COPD Risk Assessment
Risk Level
Estimated Risk Percentage
Risk Factors
Recommendations
When you light up a cigarette, you’re not just inhaling nicotine-you’re flooding your lungs with a cocktail of toxic chemicals that can set the stage for chronic obstructive pulmonary disease. This article breaks down exactly how that happens, what signs to watch for, and what you can do to protect your breathing.
Quick Takeaways
- Smoking is the leading risk factor for COPD, accounting for about 85% of cases worldwide.
- Both emphysema and chronic bronchitis are direct results of repeated exposure to tobacco smoke.
- Spirometry is the gold‑standard test for diagnosing airflow limitation.
- Quitting smoking can halt disease progression and improve quality of life, even after diagnosis.
- Pulmonary rehabilitation and proper medication management are essential for long‑term control.
How Smoking Damages the Lungs
Smoking is a chronic exposure to over 7,000 chemicals, including tar, carbon monoxide, and formaldehyde. When these substances reach the tiny airways, they trigger inflammation, oxidative stress, and mucus hyper‑production. Over time, the airway walls thicken, cilia (the tiny hairs that clear debris) become paralyzed, and the alveolar walls break down.
The damage isn’t uniform. Some smokers develop emphysema, a condition where the alveoli lose elasticity and merge, reducing surface area for gas exchange. Others end up with chronic bronchitis, characterized by a persistent cough and excess mucus.
Most patients experience a mix of both, which together form the clinical picture of COPD.
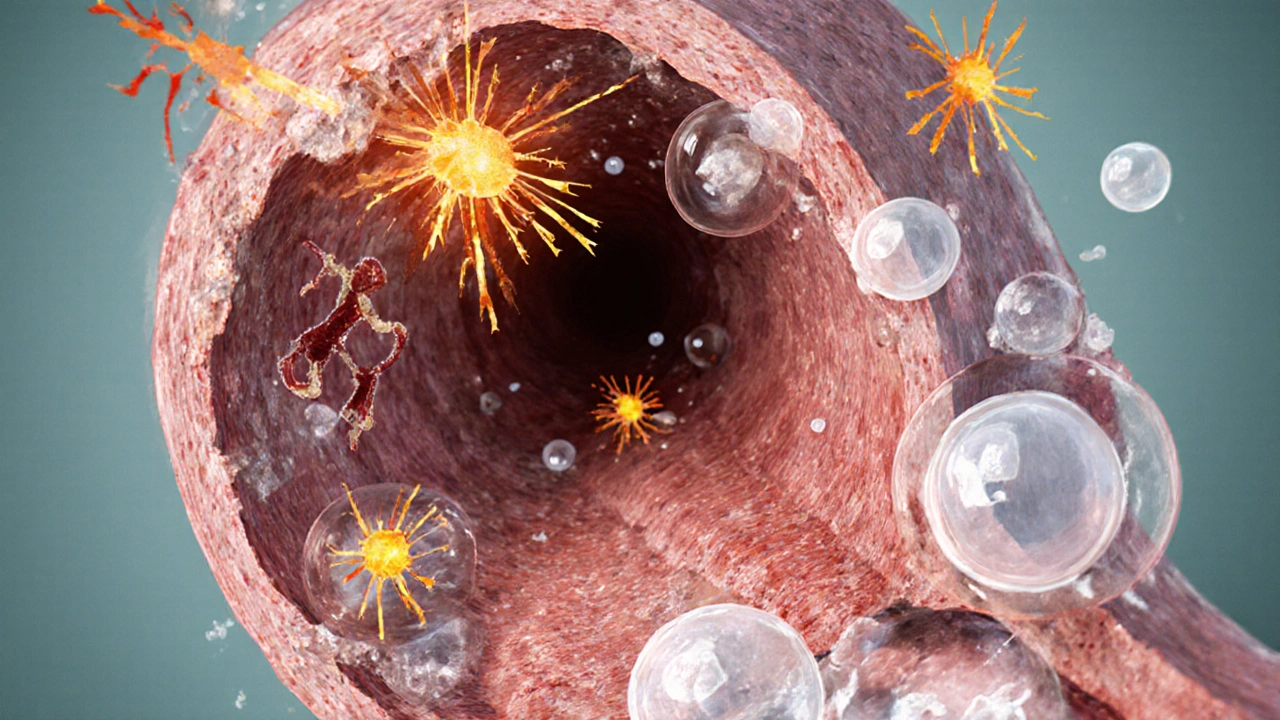
Pathophysiology of COPD
To understand why smoking leads to COPD, think of the lungs as a sponge surrounded by a network of tiny tubes. Repeated smoke exposure triggers three key processes:
- Inflammatory cascade: Immune cells such as neutrophils and macrophages flood the airways, releasing enzymes that degrade tissue.
- Oxidative damage: Free radicals in tobacco smoke overwhelm antioxidant defenses, accelerating cellular aging.
- Protease‑antiprotease imbalance: Enzymes that normally remodel lung tissue become overactive, destroying the elastic fibers that keep airways open.
These mechanisms shrink the airway lumen, increase airway resistance, and permanently limit airflow - the hallmark of COPD.
Symptoms and Diagnosis
Early COPD can be sneaky. Many smokers dismiss a mild shortness of breath as “just being out of shape.” The classic triad includes:
- Persistent cough, often worse in the morning.
- Increased sputum production.
- Gradual breathlessness during everyday activities.
If you notice any of these, talk to a doctor about spirometry. The test measures forced expiratory volume in one second (FEV1) and forced vital capacity (FVC). A post‑bronchodilator FEV1/FVC ratio below 0.70 confirms airflow limitation.
Imaging, such as a high‑resolution CT scan, can also reveal emphysematous changes that are invisible on a chest X‑ray.
Managing COPD for Smokers
Once COPD is confirmed, the treatment roadmap focuses on three pillars: symptom relief, slowing disease progression, and enhancing quality of life.
| Strategy | What It Does | Typical Example |
|---|---|---|
| Bronchodilators | Relax airway muscles to improve airflow. | Short‑acting beta‑agonists (e.g., albuterol) |
| Inhaled corticosteroids | Reduce inflammation, lower exacerbation risk. | Fluticasone propionate |
| Pulmonary rehabilitation | Exercise, education, and breathing techniques. | 6‑week supervised program |
| Vaccinations | Prevent respiratory infections that trigger flare‑ups. | Annual flu shot, 5‑year pneumococcal vaccine |
Among these, pulmonary rehabilitation often yields the biggest jump in daily stamina, especially for former smokers who regain lung muscle strength.
Quitting Smoking: The Most Powerful Intervention
Stopping smoking is the single most effective way to slow COPD progression. Within weeks, carbon monoxide levels drop, and cilia begin to recover. Long‑term, the rate of FEV1 decline can fall from 60mL/year to as low as 30mL/year.
Here’s a practical quitting roadmap:
- Set a quit date: Choose a realistic day within the next two weeks.
- Identify triggers: Stress, alcohol, or after meals often spark cravings.
- Use evidence‑based aids: Nicotine replacement therapy (patches, gum), varenicline, or bupropion improve success rates by up to 40%.
- Patch provides steady nicotine delivery for 24hours.
- Gum offers rapid relief for sudden cravings.
- Seek support: Counselors, quitlines, or smartphone apps provide accountability.
- Australia’s Quitline offers free 24‑hour coaching.
- Monitor progress: Breath‑holding tests or exhaled carbon monoxide meters can show tangible improvements.
Even if you’ve smoked for decades, quitting can add years to your life and improve daily comfort.
Risk Comparison: Smokers vs. Non‑Smokers
| Group | Lifetime COPD Risk | Typical Age of Diagnosis |
|---|---|---|
| Current smokers (≥20 pack‑years) | ~30‑40% | 50‑60years |
| Former smokers (quit ≥5years) | ~15‑20% | 55‑65years |
| Never‑smokers | ~5‑7% | 60‑70years |
The table underscores that quitting dramatically reduces risk, even if lung damage has already begun.
Preventive Strategies Beyond Quitting
Even if you’re not ready to quit, lowering exposure can help. Consider these steps:
- Switch to nicotine‑free e‑cigarettes only as a temporary bridge (though evidence is mixed).
- Avoid secondhand smoke at home or work.
- Maintain a healthy diet rich in antioxidants-fruits, leafy greens, and omega‑3 fatty acids can combat oxidative stress.
- Stay physically active; regular aerobic exercise improves overall lung capacity.
Regular health check‑ups with spirometry screening are advised for anyone with a ≥10‑pack‑year smoking history.
Frequently Asked Questions
Can COPD be reversed if I stop smoking?
The structural damage to alveoli is permanent, but quitting stops further decline. Lung function can stabilize, and symptoms often improve within months.
How long does it take for lung function to improve after quitting?
Cilia function starts recovering in 1‑3months, and measurable FEV1 gains appear after about 1‑2years, especially when combined with pulmonary rehab.
Is secondhand smoke a significant risk for COPD?
Yes. Chronic exposure to secondhand smoke can increase COPD risk by 20‑30% and accelerate symptom onset in susceptible individuals.
What role does genetics play in COPD?
Alpha‑1 antitrypsin deficiency is a rare inherited condition that predisposes to early‑onset emphysema, even in non‑smokers. However, genetics account for a small fraction of cases compared with smoking.
Are there any new medications for COPD?
Long‑acting muscarinic antagonists (LAMA) combined with inhaled corticosteroids have shown reduced exacerbations. Triple therapy inhalers are now common for severe cases.
Ellie Haynal
October 3, 2025 AT 05:55
Honestly, every time I see someone light up without a second thought, I feel the world is slowly slipping into a haze of indifference. Smoking isn’t just a personal choice; it’s a collective betrayal of the planet and future generations. The chemicals spewing into our lungs are like tiny saboteurs, eroding the very breath we take for granted. If you love your kids, your grandparents, the trees that shade your neighborhood, put the pack down. It’s not just about you-it’s about the silent suffering of every person who has to inhale that polluted air because you decided to enjoy a nicotine buzz.
Jimmy Gammell
October 13, 2025 AT 07:31
Yo, great breakdown! 👍 If you’re thinking about quitting, start with setting a quit date and tell your friends – accountability works magic. Grab some nicotine gum or patches and keep busy with a new hobby. You got this!
fred warner
October 23, 2025 AT 09:07
What an informative post! The way you described the inflammatory cascade really highlights how smoking accelerates tissue breakdown. Keep spreading the word; knowledge is the first step toward healthier lungs.
Veronica Mayfair
November 2, 2025 AT 09:43
Love the vibe of this article! 🌟 It’s cool how you threw in the quick‑take bullets-makes it super easy to scan. Also, the emoji‑friendly tone keeps it from feeling like a lecture. 🙌
Rahul Kr
November 12, 2025 AT 11:19
Interesting stuff. 😐 I think the best part is the reminder that even small changes, like avoiding secondhand smoke, can add up.
Anthony Coppedge
November 22, 2025 AT 12:55
First, kudos for the clear structure-headings, tables, and the risk calculator all work together nicely. Second, the emphasis on pulmonary rehabilitation cannot be overstated; many patients overlook exercise as a therapy. Third, note that inhaled corticosteroids should be paired with bronchodilators for optimal effect. Fourth, vaccination schedules are crucial, especially flu shots before winter. Fifth, regular spirometry can track the progression of FEV1 decline. Sixth, consider the role of diet-antioxidant‑rich foods help counteract oxidative stress. Seventh, mental health support is essential; COPD patients often experience anxiety. Eighth, tele‑health options now make follow‑up appointments more accessible. Ninth, community support groups provide peer motivation. Tenth, never underestimate the power of a solid quit‑line program. Eleventh, nicotine replacement therapy should be tailored to individual cravings. Twelfth, varenicline has shown higher cessation rates in studies. Thirteenth, bupropion can be an alternative for those with contraindications. Fourteenth, tracking exhaled carbon monoxide offers tangible feedback. Fifteenth, celebrate milestones-each smoke‑free day is a victory.
Joshua Logronio
December 2, 2025 AT 14:31
They’re hiding the real cure from us.
Nicholas Blackburn
December 12, 2025 AT 16:07
Honestly, the data you presented is spot‑on, but the way you gloss over the fact that many pharmaceutical companies push unnecessary inhalers is infuriating. People need to be skeptical about the profit motive behind those “triple therapy” combos.
Dave Barnes
December 22, 2025 AT 17:43
One could argue that the very notion of “risk calculators” mirrors a deeper philosophical question: are we quantifying health to control us? Numbers are seductive, but they also reduce human experience to cold percentages. Still, the practical utility of the tool can’t be denied.
Kai Röder
January 1, 2026 AT 19:19
Thank you for the thorough explanation. For anyone seeking guidance, consider discussing these strategies with a primary care physician to tailor a plan that fits your unique health profile.
Brandi Thompson
January 11, 2026 AT 20:55
Reading through this article feels like peeling back layer after layer of a complex onion, each slice revealing more of the tragic reality faced by smokers and, frankly, the complacent society that enables it. First, the sheer number of toxic chemicals-over 7,000-introduced into the lungs with each puff is staggering, and it’s not just nicotine that does the damage; tar, carbon monoxide, and formaldehyde each play a role in a cascade of inflammation that never truly resolves. Second, the inflammatory cascade described, with neutrophils and macrophages releasing proteolytic enzymes, is a perfect illustration of how the body’s own defense mechanisms can become weapons against itself. Third, oxidative stress, driven by free radicals from smoke, overwhelms antioxidant defenses, accelerating cellular aging and contributing to the protease‑antiprotease imbalance that ultimately destroys alveolar walls; this is the hallmark of emphysema, which is irreversible. Fourth, the article’s emphasis on the protease‑antiprotease imbalance underscores why genetic factors like alpha‑1 antitrypsin deficiency, while rare, become catastrophic in the presence of smoke. Fifth, the data on pack‑years and risk percentages is a sobering reminder that the damage is dose‑dependent, yet many people cling to the hope that “just a few more cigarettes won’t hurt.” Sixth, the discussion of spirometry as the gold‑standard diagnostic tool is crucial, because early detection can halt progression, but only if patients actually get tested-something many never do due to lack of symptoms or access. Seventh, the mention of high‑resolution CT scans adds a layer of diagnostic precision, yet it also highlights disparities in healthcare: not everyone can afford such imaging. Eighth, the treatment pillars-bronchodilators, inhaled steroids, pulmonary rehab-are essential, but they are often underutilized; pulmonary rehabilitation, in particular, can dramatically improve quality of life, yet referral rates remain low. Ninth, the emphasis on vaccination is a practical point that can prevent exacerbations, which are often the catalyst for hospitalizations and accelerated decline. Tenth, the quitting roadmap is perhaps the most empowering section, laying out concrete steps-setting a quit date, identifying triggers, using pharmacologic aids, seeking support-each backed by evidence. Eleventh, the psychological component of quitting, such as counseling and peer support, cannot be overstated; the mental battle is as fierce as the physical addiction. Twelfth, the risk comparison table starkly shows that never‑smokers still carry a baseline risk, reinforcing that environmental factors like air pollution also play a role. Thirteenth, the brief mention of e‑cigarettes as a “temporary bridge” is controversial; evidence is mixed, and this nuance should be explored further. Fourteenth, the FAQs address common concerns, but the answer about “reversal” could be more nuanced: while structural damage is permanent, functional improvement is possible, especially with rehab. Finally, this piece succeeds in weaving together pathophysiology, clinical guidance, and public health messaging, presenting a comprehensive view that should motivate both clinicians and patients to act decisively against the scourge of COPD.
Chip Hutchison
January 21, 2026 AT 22:31
Great job breaking everything down into bite‑size pieces. If you’re reading this and thinking about quitting, remember you’re not alone-many community programs are available, and they can really boost your confidence.
Emily Moody
February 1, 2026 AT 00:07
Patriotic fact: nothing undermines the American spirit like inhaling poison. Smoking is a betrayal of our nation’s vigor, an affront to the freedom we cherish. If you truly love this country, ditch the habit and stand tall like the eagle!
Tim Ferguson
February 11, 2026 AT 01:43
Sure, the article is thorough, but you can’t ignore the simple truth: quitting is a personal choice. No amount of data will force anyone if they don’t want to.
Noah Cokelaere
February 21, 2026 AT 03:19
Oh, so now we need a risk calculator for everything? Next, we’ll have an app that tells us how sad we look when we cough. 🙄